Metatarsalgia is pain and inflammation in the ball of your foot. Potential causes of the condition include foot deformities, inflammatory issues and wearing ill-fitting shoes. The pain can be intense, but at-home treatment options like rest and ice can usually clear it up. Reach out to your healthcare provider if your pain persists.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
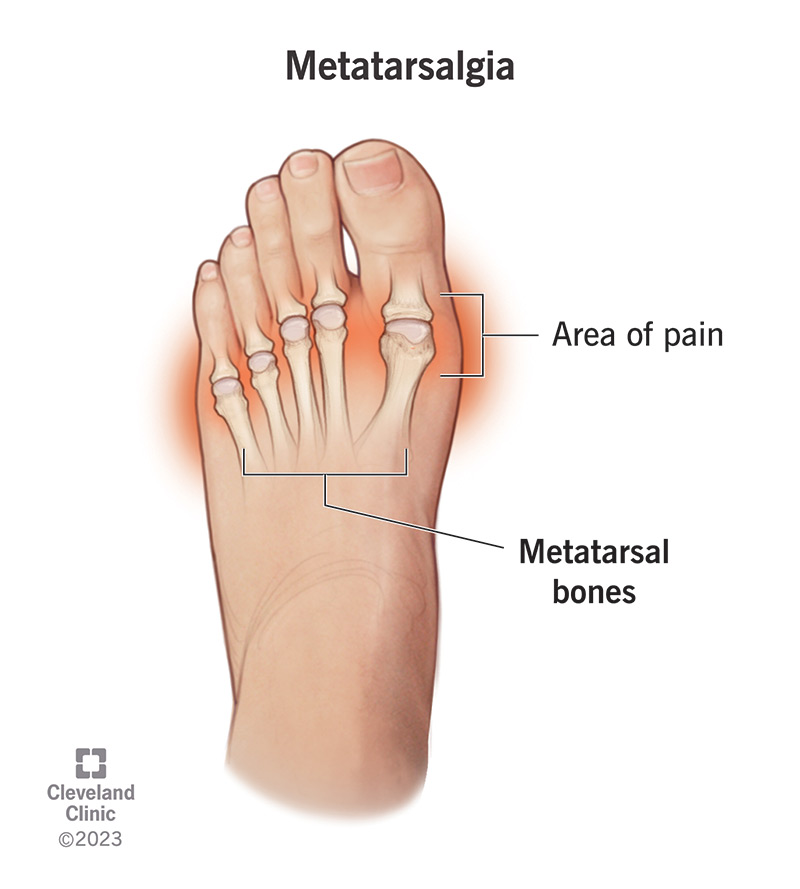
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/metatarsalgia)
Metatarsalgia (pronounced “MET-ah-tar-SAL-gee-ah”) refers to pain and inflammation in the ball of your foot, or forefoot. This is the area between the arches and toes on the bottom of your foot. The pain of metatarsalgia typically centers under one or more of the five bones at the bases of your toes, the metatarsal heads.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Metatarsalgia has a number of different causes, including:
Treatment varies depending on your condition, but typically starts with simple measures like rest, stretches and over-the-counter (OTC) pain medications.
The main symptom of metatarsalgia is pain in the metatarsal area under the ball of your foot. The condition may or may not be accompanied by swelling or inflammation. Metatarsalgia symptoms can come on quickly or develop over time. They include:
You may develop metatarsalgia if you participate in activities that involve jumping or running. Other causes of the condition include foot deformities and wearing shoes that are too high-heeled, too soft, unsupportive or overworn.
Foot and ankle surgeons divide metatarsalgia causes into three groups: primary, secondary and iatrogenic.
You can develop primary metatarsalgia if there’s an issue with your metatarsals that affects their relationship with other parts of your foot. Examples include:
Advertisement
Secondary metatarsalgia can happen if you have health issues or do activities that increase pressure on your forefoot. Examples include:
Iatrogenic metatarsalgia is a complication of forefoot surgery. For example, bunion surgery may lead to changes in your big toe that cause metatarsalgia pain. Other complications include broken bones (fractures) that don’t heal properly (or at all) and avascular necrosis. While rare, these complications can occur.
Anyone can get metatarsalgia, although runners and others who take part in high-impact sports or spend more time on their forefeet have the condition more frequently than others.
People who wear shoes that are ill-fitting, or don’t wear shoes when they need support (for example, when exercising, walking up and down stairs, or using ladders) experience metatarsalgia more than others. Also, wearing high-heeled shoes puts extra pressure on your metatarsals and heels.
In addition, people who have foot deformities and preexisting inflammatory conditions are more likely to have metatarsalgia pain.
If you have any ongoing symptoms of metatarsalgia, you should see your healthcare provider. Untreated metatarsalgia can lead to other foot and ankle conditions that can cause you to limp. Metatarsalgia can also cause pain in other parts of your body, including your lower back and hip when you compensate and begin to walk abnormally.
Your healthcare provider will begin an exam for metatarsalgia by asking about your symptoms. They’ll also examine your foot manually. You may need a foot X-ray to rule out stress fractures or other problems that could be causing your pain. Other times, they may order an ultrasound or MRI (magnetic resonance imaging) to assess the soft tissues surrounding your metatarsophalangeal joints.
Metatarsalgia treatment starts conservatively. That means your healthcare provider will want to avoid invasive measures like surgery and try simple, cautious options first. Treatment options may include:
Advertisement
If these measures don’t help relieve your metatarsalgia, your provider may recommend an injection or surgery to resolve the underlying cause of your pain.
If you have metatarsalgia, you may have severe pain and inflammation in your foot. The pain may come on quickly or develop over time. You may experience other symptoms, as well.
The first thing you’ll want to do is rest your foot. Don’t participate in any activities or sports that you think may have caused the pain. If possible, don’t stand for too long or walk too much. Avoid wearing unsupportive footwear. Avoid walking in your stocking feet for long periods of time.
With some basic measures, you should be able to treat metatarsalgia yourself and be on your way. If the pain continues after at-home treatment, you’ll want to see your healthcare provider for further evaluation.
You can’t prevent all cases of metatarsalgia, but there are ways you can avoid developing it. You may be able to prevent metatarsalgia by:
Advertisement
You can usually treat metatarsalgia at home, but you should see your healthcare provider if:
If you notice any of the following signs, you should go to the emergency room immediately. You may have a more severe injury, like a broken bone.
Questions you may want to ask your provider about metatarsalgia include:
Metatarsalgia pain can be intense. It can make it difficult for you to enjoy the things you love. You may not even be able to walk. Luckily, you can usually treat the condition yourself with some simple at-home measures. If rest and a new pair of shoes don’t do the trick, reach out to your healthcare provider. They can evaluate your symptoms and determine if you need more extensive treatment.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From sudden injuries to chronic conditions, Cleveland Clinic’s orthopaedic providers can guide you through testing, treatment and beyond.
