The Whipple procedure (pancreaticoduodenectomy) is a surgical operation to treat pancreatic cancer at the “head” of your pancreas. It removes part of your pancreas and your duodenum (the top part of your small intestine). It also removes your gallbladder and bile duct.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
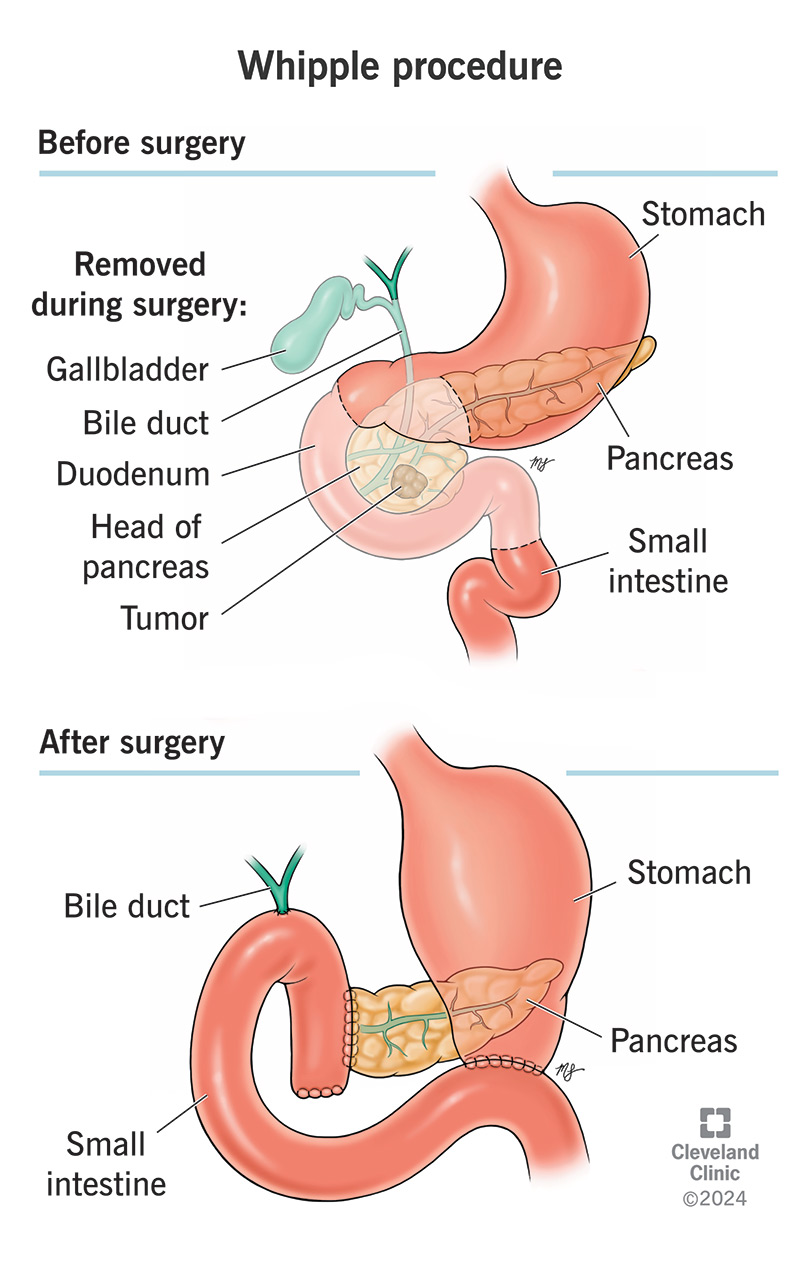
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21650-whipple-procedure.jpg)
The Whipple procedure is a complex surgery to remove cancer located at the “head” of your pancreas. This is an important junction point in your digestive system, where several organs meet. Cancer in any of these organs can spread to the others. So, the Whipple procedure removes the head of your pancreas along with other parts the cancer might spread to. These include your:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The term “pancreaticoduodenectomy” means removing part or all of your pancreas and duodenum. But surgeons understand that removing these parts also means removing other parts that are connected to them. This offers the best hope of rooting out cancer in this area. After removing all these parts, your surgeon will reconnect the remaining parts so that your digestive system can continue to function.
Surgeons (most recently, Whipple) developed the pancreaticoduodenectomy procedure to remove pancreatic cancer and other cancerous tumors near the head of your pancreas. These might include:
Occasionally, your healthcare provider might recommend the Whipple procedure to treat another condition that affects the whole area. For example, chronic pancreatitis may also affect other organs.
Advertisement
The Whipple procedure might not be appropriate for you if:
The modified Whipple procedure (pylorus-sparing Whipple) leaves your stomach intact. This might be an option if your condition doesn’t appear to involve your stomach. Because it leaves your pylorus intact, the modified Whipple procedure is less likely to affect your stomach function afterward. Surgeons choose this option whenever possible.
Before scheduling your Whipple procedure, your healthcare team will:
You’ll spend five to eight hours in surgery for the Whipple procedure. You’ll have general anesthesia, so you’ll sleep through it. Your anesthesiologist will also use additional pain-blocking techniques to keep you comfortable during surgery. These may include nerve blocks and/or pain killers through an IV line. Your surgical team will monitor your vital signs and other important health indicators continuously.
You may have:
Your surgeon will:
Advertisement
If you’re eligible for the Whipple procedure, it’s your best chance of surviving the type of cancer you have. Only about 20% of people diagnosed with pancreatic cancer can treat it effectively with surgery. That’s because this type of cancer is hard to catch in the early stages. Surgery only works if the cancer hasn’t already spread (metastasized). But if you can remove it all, you may stop it from spreading.
But the Whipple procedure does have its own risks and side effects. Recovery can be long and complicated. Your digestive system may take months to adjust and may never be the same. Most complications are temporary and treatable. But some can be lasting and affect your quality of life. And even if you don’t have any complications, the procedure can’t guarantee that you’ll survive cancer.
Complications of the Whipple procedure can include:
Advertisement
You’ll spend a week to two weeks recovering in the hospital after surgery. You’ll have pain relief as needed. You may need to be fed through a tube or through an IV while your digestive system heals. In the meantime, your healthcare team will run tests to try to determine if they removed all the cancer. Depending on what they find, they might suggest additional treatments after you’ve fully recovered.
Most people can return to their activities after about six weeks. But it may take several months before you feel fully recovered. You might feel very tired during this time. Many people find they can eventually return to eating normally. But others might need long-term changes. If you have continuing digestive difficulties, talk to your provider. It’s important to get adequate nutrition while you’re recovering.
Current survival rates related to the Whipple procedure range from 97% to 99%. Survival rates after the procedure depend on the type of cancer you have, the stage and other factors. Most people who have the Whipple procedure can increase their life expectancy to some degree. When cancer has spread to nearby lymph nodes or other areas, the five-year survival rate after surgery is between 20% and 25%.
Advertisement
Pancreatic cancer is a devastating diagnosis — like a massive storm cloud that shadows every step you take. And you know it’s only a matter of time until it rains enough to cover your whole world. The Whipple procedure is a silver lining, offering hope for brighter days. Remember, you’re not alone. Lean on the support of your loved ones and reach out to your healthcare provider for any resources and assistance you need.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Sometimes you have surgery planned. Other times, it’s an emergency. No matter how you end up in the OR, Cleveland Clinic’s general surgery team is here for you.
