Thyroiditis represents a group of conditions that cause inflammation of your thyroid gland. Hashimoto's thyroiditis is the most common type. Some cases of thyroiditis are temporary and others cause permanent hypothyroidism (underactive thyroid). It’s treatable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
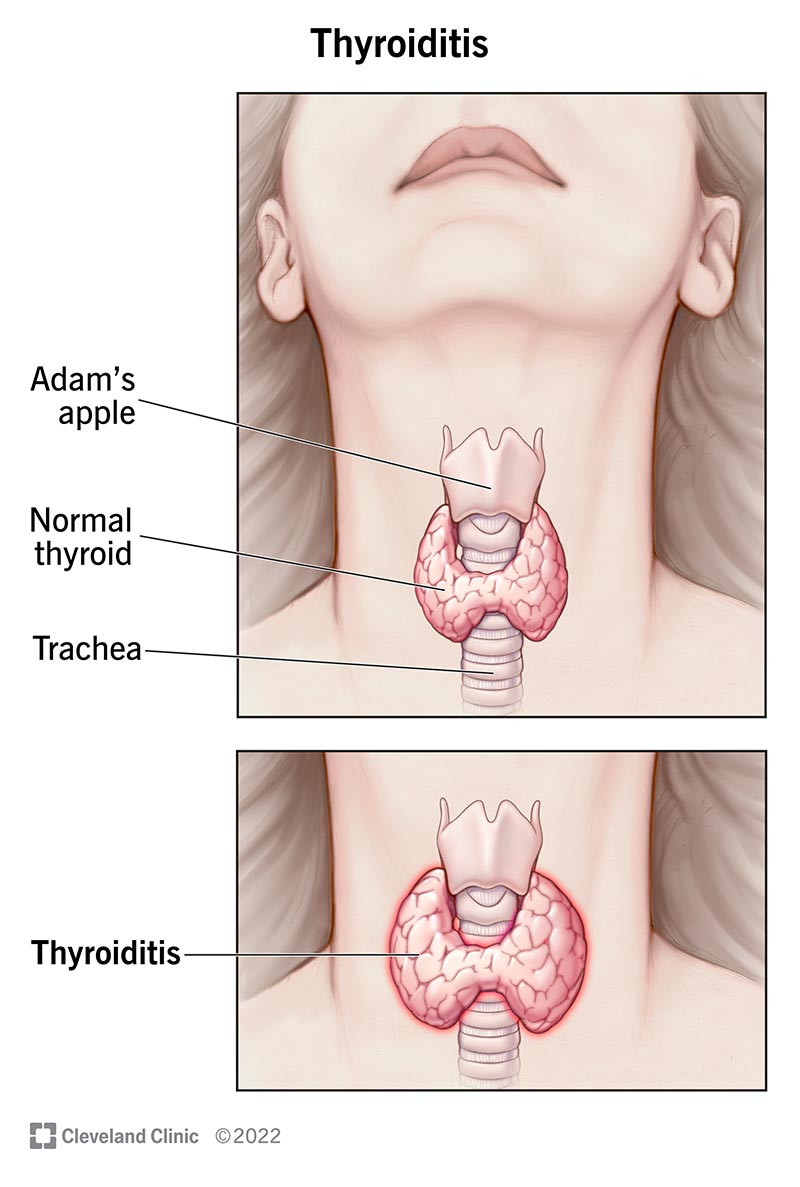
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15455-thyroiditis)
Thyroiditis is inflammation of your thyroid gland. Your thyroid is a small, butterfly-shaped gland located at the front of your neck under your skin. It’s a part of your endocrine system and controls many of your body’s important functions by producing and releasing certain hormones.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Thyroiditis includes a group of individual conditions that cause thyroid inflammation but have different causes and symptoms. Thyroiditis can lead to over- or under-production of thyroid hormone.
In most types of thyroiditis, there are three phases, including:
Types of thyroiditis include:
Advertisement
Thyroiditis can affect anyone, but it more commonly affects women.
Hashimoto’s thyroiditis is four to 10 times more common in women. It most often develops between the age of 30 to 50.
Silent or painless thyroiditis is also common in women and is the next common cause of thyroiditis after Hashimoto’s thyroiditis.
The most common form of thyroiditis is Hashimoto’s thyroiditis, which affects approximately 1% to 2% of people in the United States. The other types of thyroiditis are rarer.
Thyroiditis generally isn’t life-threatening.
However, a life-threatening condition called thyroid storm can develop if you have long-term untreated or undertreated hyperthyroidism, which can develop from thyroiditis.
Symptoms of thyroid storm include:
If you’re experiencing these symptoms, call 911 or get to the nearest hospital as soon as possible.
If you’re experiencing symptoms of thyroiditis, it’s important to talk to your healthcare provider so they can order tests to diagnose it and treat it.
The symptoms of thyroiditis depend on the type of thyroiditis and its phase. Most types of thyroiditis cause thyrotoxicosis symptoms followed by hypothyroid symptoms.
Subacute thyroiditis and acute infectious thyroiditis usually also cause pain in your thyroid area. Some people with thyroiditis have an enlarged thyroid gland (goiter).
The thyrotoxic phase of thyroiditis is usually short, lasting one to three months. If your thyroid cells are damaged quickly and there’s a leak of excess thyroid hormone, you might experience symptoms of hyperthyroidism (overactive thyroid), which include:
The hypothyroid phase of thyroiditis can be long-lasting and may become permanent. If your thyroid cells are damaged and thyroid hormone levels fall, you might experience the symptoms of hypothyroidism, which include:
Thyroiditis is caused by an attack on your thyroid, causing inflammation (your body’s response to an injury) and damage to the thyroid cells. It has several different causes depending on the type.
The most common cause, or “attacker,” is an autoimmune disease, which is the result of your immune system accidentally attacking your body instead of protecting it. It's unclear why your immune system does this. Antibodies that attack your thyroid cause most types of thyroiditis.
Advertisement
This chart lists the causes for each type of thyroiditis.
| Type of thyroiditis | Cause |
|---|---|
| Hashimoto’s thyroiditis | Antithyroid antibodies, autoimmune disease. |
| Silent or painless thyroiditis | Antithyroid antibodies, autoimmune disease. |
| Postpartum thyroiditis | Antithyroid antibodies, autoimmune disease. |
| Subacute thyroiditis (de Quervain’s thyroiditis) | Likely a virus. |
| Acute infectious thyroiditis | Most commonly bacteria, but any infectious organism. |
| Radiation-induced thyroiditis | Follows treatment with radioactive iodine for hyperthyroidism or external beam radiation therapy for certain cancers. |
| Drug-induced thyroiditis | Certain medications, including amiodarone, lithium, interferons, interleukin-2 and checkpoint inhibitors. |
| Riedel thyroiditis | Fibrosis (thickening and scarring) of your thyroid. |
| Type of thyroiditis | |
| Hashimoto’s thyroiditis | |
| Cause | |
| Antithyroid antibodies, autoimmune disease. | |
| Silent or painless thyroiditis | |
| Cause | |
| Antithyroid antibodies, autoimmune disease. | |
| Postpartum thyroiditis | |
| Cause | |
| Antithyroid antibodies, autoimmune disease. | |
| Subacute thyroiditis (de Quervain’s thyroiditis) | |
| Cause | |
| Likely a virus. | |
| Acute infectious thyroiditis | |
| Cause | |
| Most commonly bacteria, but any infectious organism. | |
| Radiation-induced thyroiditis | |
| Cause | |
| Follows treatment with radioactive iodine for hyperthyroidism or external beam radiation therapy for certain cancers. | |
| Drug-induced thyroiditis | |
| Cause | |
| Certain medications, including amiodarone, lithium, interferons, interleukin-2 and checkpoint inhibitors. | |
| Riedel thyroiditis | |
| Cause | |
| Fibrosis (thickening and scarring) of your thyroid. |
Your healthcare provider will perform a physical exam, including assessing your thyroid, and ask you questions about your symptoms and medical history.
If they suspect you may have thyroiditis after, they’ll likely order any combination of the following tests to help diagnose it:
Advertisement
The treatment for thyroiditis depends on the type and the symptoms.
If you’re in the thyrotoxic phase of thyroiditis, your provider may prescribe beta-blockers to decrease palpitations (fast heart rate) and tremors.
As your symptoms improve, your provider will taper off the medication since the thyrotoxic phase is temporary.
If you have Hashimoto’s thyroiditis, your provider will prescribe thyroid hormone replacement medication, such as levothyroxine. You’ll likely have to take this medication for the rest of your life since the hypothyroidism from Hashimoto’s thyroiditis is usually permanent.
If you have subacute, painless (silent) or postpartum thyroiditis and have hypothyroid symptoms, your provider will prescribe thyroid hormone replacement medication. You’ll likely have to take the medication for approximately six to 12 months and then taper off it to see if you have permanent hypothyroidism or not.
If the hypothyroidism is mild and you have few, if any, symptoms, then no medication may be necessary.
If you have acute infectious thyroiditis, the infection will need to be treated. This will likely involve antibiotics. If an abscess forms on your thyroid, your provider may need to drain the fluid and pus with fine-needle aspiration (needle biopsy).
Advertisement
Drug-induced thyroiditis usually lasts as long as you’re taking the medication causing it. Your provider may switch you to a different but similar medication to treat the thyroiditis or they may prescribe levothyroxine (thyroid hormone medication) while you continue to take the medication causing thyroiditis.
The pain caused by acute infectious thyroiditis and subacute thyroiditis usually can be managed with nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin or ibuprofen. In some cases, the pain can be severe and may require steroid therapy.
Riedel thyroiditis requires surgical treatment.
The prognosis (outlook) for thyroiditis is generally good.
In the case of Hashimoto's thyroiditis, the resulting hypothyroidism is generally permanent, but it’s treatable with life-long thyroid hormone replacement therapy.
People who develop subacute thyroiditis usually have symptoms for one to three months, but complete recovery of thyroid function can take up to 12 to 18 months. These people have about a 5% chance of developing permanent hypothyroidism.
Full thyroid function recovery from postpartum and silent (painless) thyroiditis also takes about 12 to 18 months. People with these conditions have about a 20% chance of developing permanent hypothyroidism.
Unfortunately, most cases of thyroiditis can’t be prevented.
If you have a condition that requires treatment using radioactive iodine or radiation therapy, talk to your healthcare provider about your risk of thyroiditis. You may be able to start with other treatments to avoid developing thyroiditis.
If you take prescription drugs that can cause thyroiditis, talk to your provider about your risk and if you can stop taking them. You still may not be able to avoid thyroiditis.
If you’ve been diagnosed with thyroiditis, you’ll need to see your healthcare provider regularly to monitor your symptoms and make sure your treatment is working.
If you develop worse or more concerning symptoms, call your provider as soon as possible.
While it’s usually stressful to learn you have a medical condition, the good news is that thyroiditis is highly treatable — and it may even be temporary. If you have any questions about thyroiditis or your treatment plan, talk to your healthcare provider. They’re available to help you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s experienced healthcare providers treat all kinds of thyroid disorders, including issues that cause hypothyroidism and hyperthyroidism.
