Postpartum thyroiditis is a relatively rare and often temporary condition where your thyroid gland becomes inflamed after a pregnancy. It affects about 5% to 10% of women within the first year of pregnancy. Those with Type 1 diabetes or a history of thyroid trouble are most likely to develop postpartum thyroiditis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Postpartum thyroiditis is a rare condition where your thyroid gland becomes inflamed within the first year after pregnancy. It’s a type of thyroiditis, or inflammation in your thyroid gland. Your thyroid is a butterfly-shaped gland in the lower front of your neck. It releases hormones that control essential body processes, including how you use energy (metabolism).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Postpartum thyroiditis usually unfolds in phases.
Not everyone experiences all the phases in order, though. Some people skip over the hypothyroid phase. They have hyperthyroidism, and then their thyroid function returns to normal.
It's rare but possible to remain in the hypothyroid phase. You’ll need hormone replacement therapy to make up for low thyroid hormone levels.
An estimated 5% to 10% of women experience postpartum thyroiditis in the year after a birth, abortion or miscarriage. Rates are higher among those with more risk factors, like a thyroid condition.
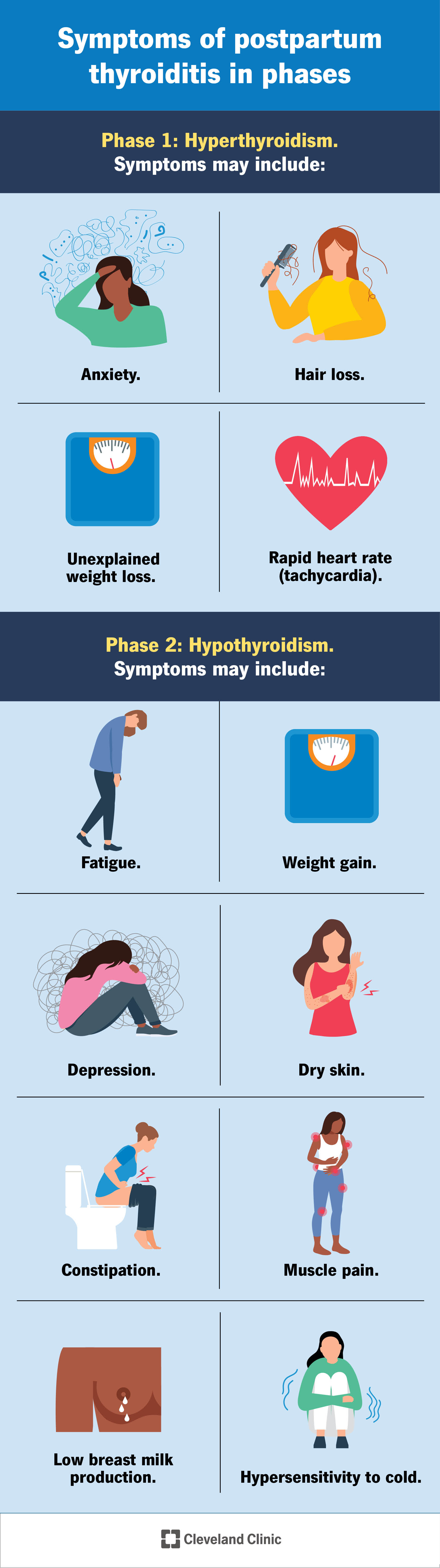
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/15294-postpartum-thyroiditis.jpg)
It's common not to notice symptoms in the first phase, hyperthyroidism. If you do experience symptoms, they usually involve body functions (like metabolism) being “hyper” or sped up. They may include:
Advertisement
It isn’t until the second phase, hypothyroidism, that most people notice symptoms. Symptoms of hypothyroidism usually involve body functions (like metabolism) slowing down. They may include:
Postpartum thyroiditis involves anti-thyroid antibodies attacking your thyroid gland. Antibodies are your body’s protectors. They fight germs that make you sick. With postpartum thyroiditis, antibodies go haywire and attack your thyroid gland instead. The attack causes inflammation in your thyroid.
The process is like what happens in Hashimoto’s disease, which is the most common type of thyroiditis.
Scientists are still researching what causes the antibodies to attack after a pregnancy. A popular theory is that you’re more likely to get diagnosed if you had an underlying autoimmune condition (that you didn’t know about) before pregnancy. An autoimmune condition happens when antibodies attack healthy cells and tissue.
You’re more likely to develop postpartum thyroiditis if you:
Your healthcare provider will perform a physical exam and ask about your symptoms. They’ll do a blood test to check the levels of thyroid hormones (T3, T4 or TSH) in your blood. A blood test is usually enough to diagnose postpartum thyroiditis. It can also help exclude similar diagnoses, like Graves’ disease.
Graves’ disease is a lifelong condition that causes symptoms similar to postpartum thyroiditis.
Most women have mild symptoms and don’t need treatment unless symptoms worsen. If your symptoms are severe, you’ll need prescription medications. Let your provider know if you’re breastfeeding. They can recommend medications that are safe for you and your baby.
Treatment depends on whether you’re experiencing hyperthyroidism or hypothyroidism.
Advertisement
Your healthcare provider will monitor your thyroid levels during treatment.
Postpartum hypothyroidism is usually temporary. Seventy to 80% of those with the condition eventually no longer need medication because their thyroid starts making hormones at normal levels again. The other 20% to 30% stay in the hypothyroid phase. They’ll need thyroid long-term hormone replacement therapy.
Postpartum hypothyroidism also makes you more likely to develop future thyroid issues, including hypothyroidism or an enlarged thyroid gland (goiter). Even if your thyroid returns to normal, your provider will likely need to monitor your thyroid.
Postpartum thyroiditis usually lasts between a year and a year and a half. Usually, within 12 to 18 months from when you first notice symptoms, your thyroid will return to normal. At this point, you’ll no longer need medicine.
Absolutely. Many women go on to have healthy pregnancies after postpartum thyroiditis. It’s important, though, that you tell your provider that you’ve had this condition if you’re planning a pregnancy. Approximately 20% of individuals with a history of postpartum thyroiditis develop it during later pregnancies.
Your provider can monitor your thyroid hormone levels to help guide you through a healthy pregnancy.
Advertisement
Questions include:
Many people with postpartum thyroiditis symptoms delay seeing their provider because they assume the changes are a normal part of pregnancy recovery. Caring for an infant can cause changes that may feel like hypothyroidism symptoms, like fatigue and muscle pain. But don’t assume you have to power through symptoms that aren’t improving. The problem may be your thyroid. A simple blood test is usually all it takes, so you know for sure. There are medications that can help you feel better and more capable of managing life with a new baby.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
