Breastfeeding is when you feed your baby milk that comes from your body. Experts recommend breastfeeding as your baby’s only source of nutrition until age 6 months, whenever possible. This provides nutrients and antibodies to support your baby’s health. Your baby continues to benefit from breastmilk even after they start eating solids.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
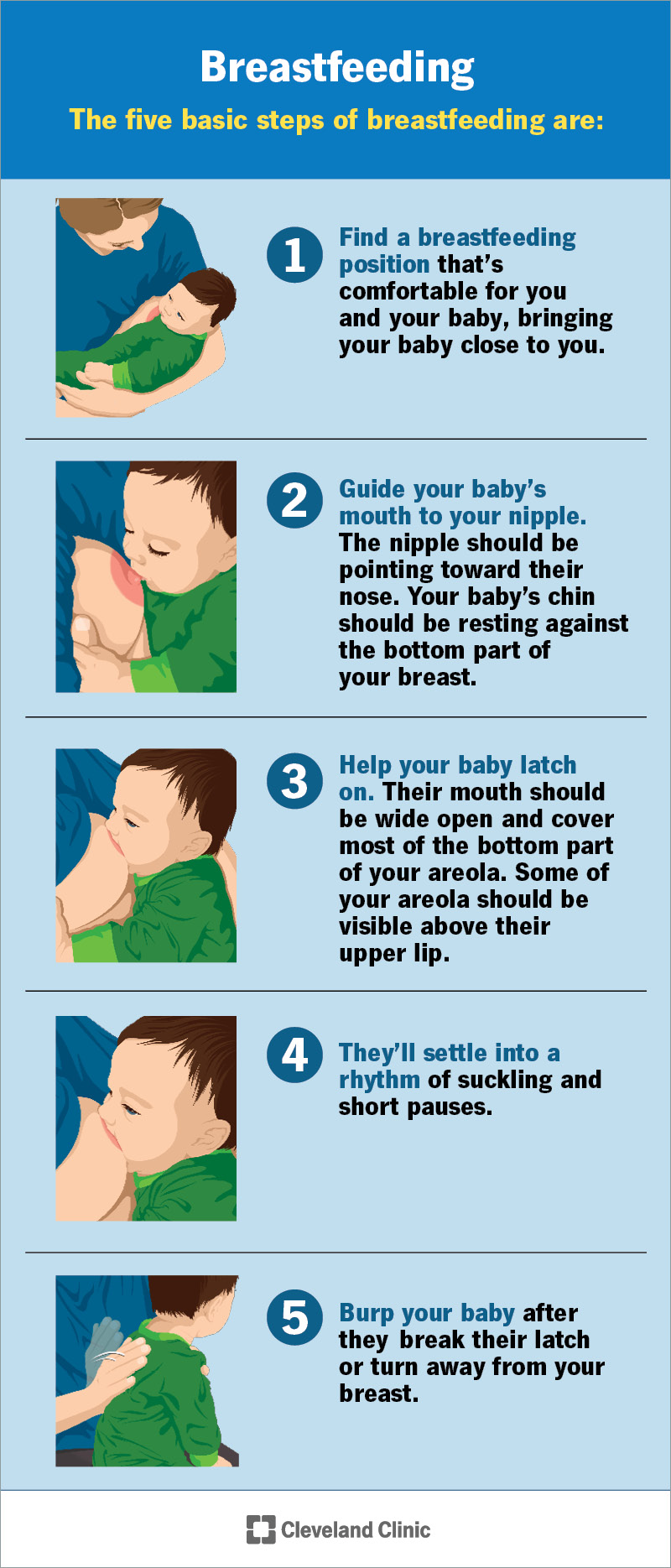
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/5182-breastfeeding.jpg)
Breastfeeding is the process of feeding your baby milk that your body has made. Your baby attaches their mouth onto your breast and, through a suckling motion, drinks milk. Your baby will likely start breastfeeding soon after birth, often within the first few hours.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
At first, your body will make an early form of milk called colostrum. This is a protein-rich, thick liquid. It’s full of antibodies that help guard your newborn against infections. Your colostrum will change into mature milk after about three to five days of breastfeeding. During this time, your baby will lose a bit of weight. This is normal. They’ll regain it once your milk “comes in.”
Breastfeeding has many benefits both for you and your baby. These include lowering your risk for postpartum depression and building your baby’s immune system.
If possible, exclusively breastfeed your baby for their first six months of life. Continue breastfeeding as you introduce solid foods. Because breastmilk has so many benefits, you can keep providing it until your baby’s second birthday or longer.
Keep in mind that there are many ways to feed your baby. You might nurse directly. You might pump milk to feed your baby with a bottle. You may breastfeed and supplement with formula. You may use only formula or donor breast milk. Your needs and your baby’s needs might change over time. What matters most is that your baby has the nutrients they need to grow and develop. Your healthcare provider can guide you on what’s best in your situation.
Advertisement
Milk makes its way from your body to your baby through a series of steps:
You might hear your provider say that lactation works on a supply and demand basis. This means your body takes cues from your baby’s “demands” to know how much milk to produce. If your baby empties your breast, your body will replenish the supply. If your baby removes less milk because they’re starting solids, your body will adjust and make less.
This is why pumping while you’re away from your baby can help you keep up your supply. When milk is removed, your body knows to make more. This is also why you shouldn’t pump to “empty your breasts” to get rid of engorgement if you have an issue with overproduction. Draining your breasts only tells your body to make more milk.
A healthcare provider will help you get started soon after delivery. If you and your baby are healthy, you’ll hold your baby against your skin for at least two hours. This is called skin-to-skin contact. This close contact encourages your baby to bond and breastfeed.
Your baby will eventually start moving toward your breast. This is an instinct, and it’s a special one for you to witness! Your provider can help make sure your baby latches on and begins taking in milk.
For every breastfeeding session after, you’ll:
The next time you feed your baby, start with the breast that wasn’t emptied as much. It’ll likely feel fuller because it contains more milk.
Advertisement
Your baby might be hungry if they:
Your baby is likely full if they:
Just like during pregnancy, you should pay attention to what you eat and drink when you’re breastfeeding. There aren’t as many restrictions when you’re breastfeeding compared to pregnancy. But there are some things to limit or avoid:
Advertisement
Yes, but you should talk with your healthcare provider about the best type for you and when to start it. In general, it’s safe to use:
Hormonal birth control methods that contain estrogen (like certain pills, patches and vaginal rings) may lower your milk supply. So, your provider may suggest you avoid them or wait at least one month after giving birth (and take the lowest possible dose).
Remember that you can still get pregnant while breastfeeding — even if you haven’t gotten a period yet.
Healthcare providers recommend breastfeeding in most situations. But you shouldn’t breastfeed if:
Some of these situations are temporary. Your provider will tell you if and when it’s safe to nurse. They’ll also explain other options for feeding your baby, like formula and donor breast milk.
Advertisement
If you run into challenges while breastfeeding — or have trouble getting started — you’re not alone. It’s common to face issues like:
The most important thing to know is that help is available. Often, these issues are solvable. Healthcare providers can help you manage any challenges so you can continue breastfeeding for as long as you’d like.
When you’re trying to learn how to breastfeed or solve a problem, you might wonder where to turn for help. You can always contact your primary care provider or obstetrician to get started. Or you may choose to see a provider with special training in breastfeeding. Examples include:
Sometimes you don’t need an expert but instead just an extra set of hands. This is where your support network can step in and help. Don’t hesitate to ask your partner or a loved one to be there with you while you breastfeed. They can grab supplies, burp your baby or just keep you company (and awake) when you need a boost.
For many, there are concerns and worries about specific aspects of breastfeeding. It’s important to remember that all questions are worth asking when it comes to caring for your child. Don’t be afraid to share whatever’s on your mind with your healthcare provider. It’s best that you get the correct information before you make important decisions about breastfeeding.
Some common questions and answers include:
No. Breast size doesn’t affect your ability to breastfeed. The amount of milk your breasts make will depend on your overall health and how much your baby eats.
Breastfeeding shouldn’t hurt. If it does, it might be because your baby isn’t latched onto your breast well. Your healthcare provider can help you learn how to hold your baby and get a good latch. If you still have pain, tell your provider so they can look for other causes.
Each person’s experience is unique. In general, breastfeeding is a learned skill and takes practice.
You might feel like you need four arms or hands to do it for the first couple of weeks. But learning to breastfeed is a bit like learning how to ride a bike. Reading the instructions can help you understand the basics, but you don’t truly learn how to do it until you’re “hands-on” and start practicing.
Many hospitals offer breastfeeding classes that you can attend during pregnancy. In most cases, nurses and lactation consultants are also available to give you information and support.
If you need to be away from your baby, you can pump or hand express your milk. Store the milk in the fridge or freezer. The person who’s staying with your baby can feed them from a bottle.
If you’re returning to work, talk to your employer about their policies for pumping breaks. In the U.S., the Fair Labor Standards Act provides you with the right to take breaks for pumping.
Pumping while you’re away from your baby serves two purposes. It allows you to store your milk to give to your baby later. It also helps you keep up your milk supply.
Breastfeeding might become one of your most cherished memories. But that doesn’t mean it always “comes naturally” or is a smooth or easy process. Don’t expect yourself to instantly know how to breastfeed. And resist the urge to blame yourself if things don’t quite go as planned.
Instead, soak up as much knowledge as you can and ask as many questions as you want. Work closely with a healthcare provider who’s specially trained in breastfeeding and lactation. They can teach you how to get started and what to do if you run into issues.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Breastfeeding is natural and rewarding, but it’s not without challenges. Get the support you need at Cleveland Clinic.
