A breast pump is a medical device that removes milk from your breasts. It allows you to maintain your milk supply when you’re away from your baby or your baby can’t breastfeed for a while. There are several types to choose from. Some pumps run on electricity or batteries and are more efficient than manual pumps.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A breast pump is a device that removes breast milk from your breasts. You may decide to use a breast pump if you’re breastfeeding and need to:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Removing (expressing) milk may become part of your daily routine. But that doesn’t mean it’s simple or that learning how to use a breast pump is intuitive. Be patient with yourself and know it might take a little time. Choosing the right pump for you can help make the process easier.
There are several types of breast pumps that each work a little differently.
With this type of pump, you squeeze a lever to create suction that helps milk come out. A manual pump takes some more work on your part, and each pumping session can take a while. However, it allows you to control the pace and rhythm of pumping, and it’s low-cost. It also doesn’t require electricity or batteries to operate and can be easily transportable.
Most manual pumps are single pumps. This means you remove milk from one breast at a time.
Advertisement
Powered pumps, unlike manual ones, use a motor to create suction and remove milk. There are two types of powered pumps: electric breast pumps and battery-powered breast pumps.
You need to plug an electric pump into a wall outlet while you use it. With a battery-powered pump, you don’t have to be near an outlet and can pump on the go. It just requires a battery that you either replace or recharge.
Some powered pumps are double pumps, meaning you can remove milk from both breasts at once. This time-saving feature is a big plus for many parents.
This is a specific type of powered pump that you tuck into your bra. Some wearables are more discreet than others. But the general idea is that you can pump while in public or on the go without people easily noticing. A wearable pump frees up your hands to do other things (you don’t have to hold the pump parts in place). So, you may like this type if you need to multitask while pumping.
This term sometimes refers to wearable pumps. But a hands-free pump can also attach to your breast and stay in place while you do other things. They don’t necessarily fit inside your bra.
You may choose to get a hands-free pumping bra. This is a piece of clothing that supports the pump and makes you more comfortable as you go about your daily tasks.
These are silicone devices that collect milk from one breast when your baby is breastfeeding on the other breast. Some use suction just like a pump to draw milk out. Some passively collect milk that would have otherwise dripped into your bra/nursing pad from letdown. If you have an oversupply of milk, speak to your provider before using.
You might be wondering, what’s the best breast pump I can get? The answer is simple: there’s no one pump that’s best for everyone. That’s because everyone has different needs and preferences. And there’s a huge variety of pumps out there to choose from.
If you’re overwhelmed by all the options and don’t know where to start, talk to a lactation consultant. They’ll help you look at the features of different pumps and decide which pump is best for you. Some questions you might want to think about include:
Your answers can help you and your lactation consultant find the best fit for your needs. For example, a powered pump may be preferable if you:
Advertisement
On the other hand, a manual pump is a good option for some people and situations. Here are some points to consider:
Your lactation consultant will discuss all these factors with you and help you reach the best decision for your needs.
Breast pump parts include:
Advertisement
These parts might look or feel a little different depending on the type of pump you have. It’s a good idea to look at and compare different pumps to get a sense of what’s out there, and what each one looks like. Your lactation consultant can also help you do this.
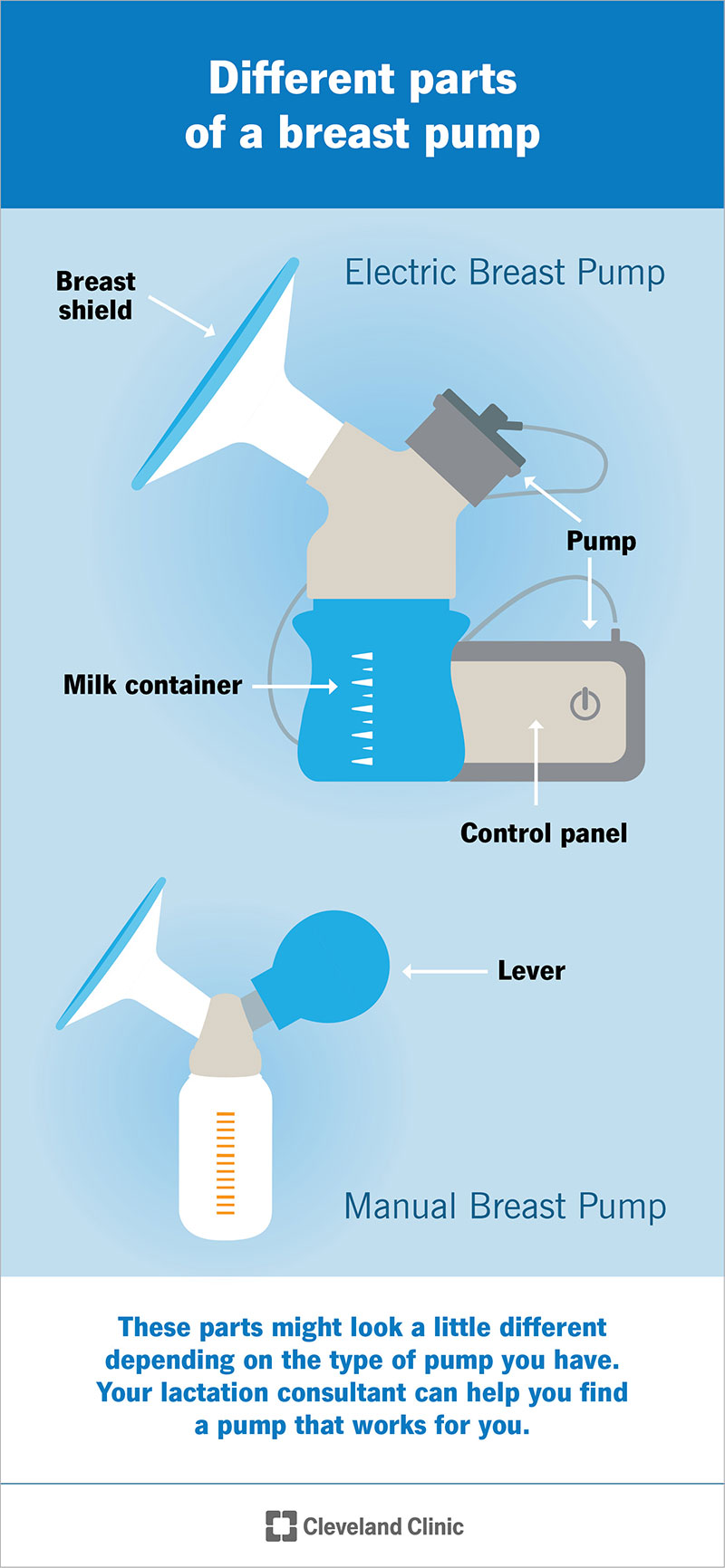
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/25244-breast-pump.jpg)
Breast pumps generally have a container for holding milk and a shield that fits onto your breast.
If you’ve never used a pump, you’re probably wondering how to pump breast milk. The specific details depend on the pump you’re using. In general, you’ll follow these steps:
Advertisement
You can safely store expressed milk for up to four days in the fridge and up to twelve months in the freezer (though using it within six months is best).
As with any new device, you might need a little time to get used to your breast pump. But your lactation consultant, friends and family can help. Online communities of parents who breastfeed or pump can also offer practical and emotional support.
Cleaning your breast pump after each use is crucial for keeping you and your baby safe from infections. Your pump’s instruction manual will tell you exactly how to clean your pump.
General steps for washing by hand include:
Your instruction manual will tell you if you can wash pump parts in the dishwasher.
In addition to washing the pump after each use, you should also sanitize it at least once a day. Sanitizing is an extra layer of protection from germs, beyond washing with soap and water. Sanitizing is crucial if your baby:
To sanitize the pump parts, follow the instruction manual’s guidelines. The manual may tell you to steam the parts in a microwave or boil them in water. Make sure you clean the pump parts first, following the steps above (never jump right to sanitizing after pumping).
You may be able to skip daily sanitizing as your baby gets older if they don’t have underlying health issues. When in doubt, ask your pediatrician about best practices.
Here are a few other things to keep in mind:
You can start pumping soon after your baby is born. But wait to give expressed milk to your baby in a bottle until they’ve gotten the hang of breastfeeding. For many babies, this takes about four to six weeks.
Giving your baby a bottle too soon can interfere with their ability to breastfeed. Healthcare providers call this “nipple confusion.” They may struggle to latch on or may turn away from your breast. Your lactation consultant can help you decide when to start pumping and when to begin bottle feeds.
Your breasts will refill with milk every time they’re emptied, so pumping can stimulate more milk production. Talk with your provider if you have any oversupply of milk.
Contact your insurance provider to find out if your plan covers a breast pump. Questions you may want to ask include:
If you have access to healthcare through the U.S. Health Insurance Marketplace, your plan is required to cover the cost of your breast pump. Your plan will describe specific details, including whether the pump is new or a rental, and whether it’s manual or powered.
It depends. There are two kinds of breast pumps:
Most of the pumps you’ll buy at the store are single-use. That means they’re meant for you and you alone, and sharing can lead to infections. Never share a single-use pump, even with family or friends. And although you can find lots of treasures at garage sales, don’t buy a single-use breast pump secondhand. This isn’t safe for you or your baby.
You can safely rent or borrow a multi-use pump from an authorized provider, like a hospital or lactation consultant. These pumps are literally just that — pumps. They don’t come with all the other parts that touch breast milk (like milk containers and flanges). Your lactation consultant or healthcare provider can tell you which parts you’ll need to purchase to use with a shared pump.
It’s good to have options, but sometimes an endless array of choices can be overwhelming. You might feel that way when choosing a breast pump. Advice from loved ones can help. But remember that the best breast pump for someone else might not be the best one for you.
That’s why it’s a good idea to talk to a lactation consultant. Tell them your plans for pumping and any special circumstances or needs (like low milk supply or flat or inverted nipples). They’ll look at the big picture as well as the little details to help you choose the right pump for you. They can also continue to support you throughout your pumping and breastfeeding journey.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Breastfeeding is natural and rewarding, but it’s not without challenges. Get the support you need at Cleveland Clinic.
