Pericardial effusion is a collection of excess fluid in your pericardium, the sac around your heart. When it happens quickly or involves a large amount of fluid, the extra fluid can take up too much space in your pericardium. This compresses your heart and interferes with how it should work. Treatment depends on how severe your condition is and what caused it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
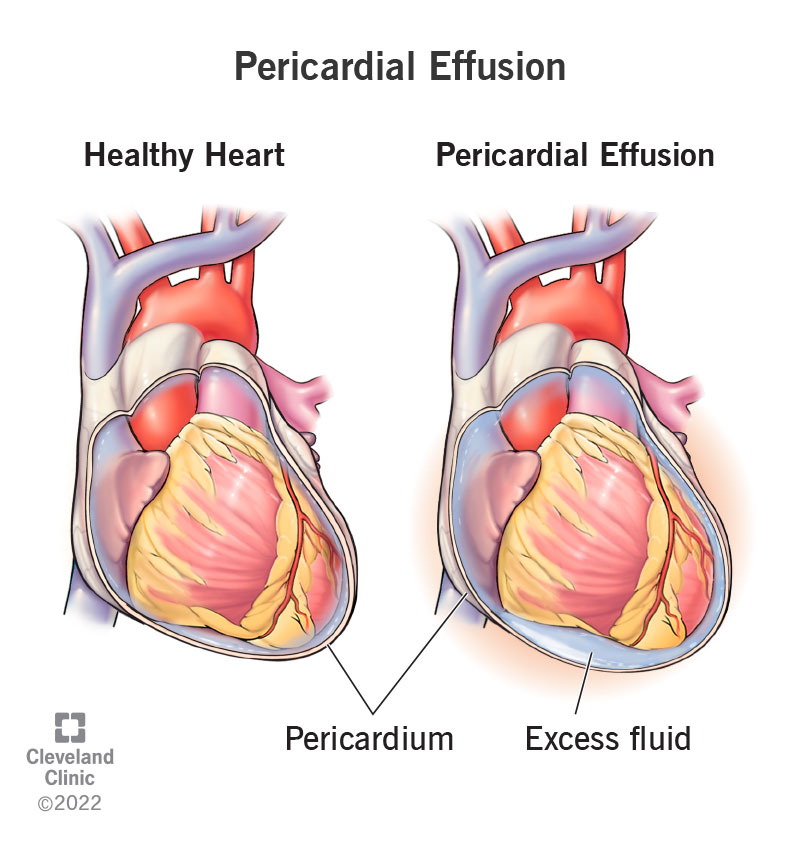
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17351-pericardial-effusion)
Pericardial effusion is a buildup of fluid in the space around your heart. It can happen for many reasons, like infections, injuries or other medical conditions. If the buildup is severe or happens quickly, it can compress your heart and cause a life-threatening medical emergency.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When a pericardial effusion happens slowly, your pericardium (the sac around your heart) has time to stretch and make room for the extra fluid. When it happens quickly, your pericardium doesn’t have time to stretch. The fluid buildup puts more and more pressure on your heart. This leaves your heart’s chambers without room to expand and fill up. Because of this, your heart pumps less blood, depriving your organs of blood flow.
An easy way to see how pericardial effusion affects your heart is by trying to blow up a balloon inside of a plastic bottle. In this example, your heart is the balloon and the bottle is the pericardium. When the bottle is empty, there’s more space for the balloon to inflate. If you add water to the bottle, there’s less space and you can’t blow up the balloon as much. If you keep filling the bottle, eventually, you can’t blow up the balloon at all.
Pericardial effusion is a relatively common condition. Because it can happen for a wide range of reasons, it can happen to people of any age or background.
A pericardial effusion can lead to cardiac tamponade. Between the inner wall of the pericardium and your heart is a thin layer of fluid. This cushions and protects your heart from outside forces (much like bubble wrap around a fragile item inside a shipping box).
Advertisement
Usually, your pericardium has just enough fluid to cushion your heart, but not so much fluid that it keeps your heart from expanding and filling up with blood. Cardiac tamponade happens when your heart has no room to expand and fill with blood. Without quick treatment, it can make your heart stop, which is eventually fatal within minutes to hours.
Cardiac tamponade is a complication of pericardial effusion, but not the only one.
As your heart pumps less and less blood, it speeds up to try to make up for its limited pumping ability. Over time, your heart can’t keep up, and you can go into cardiogenic shock. Without treatment, cardiogenic shock is fatal.
You may not have any pericardial effusion symptoms with a mild case. Symptoms are more likely when an effusion happens quickly, involves a large amount of fluid or causes cardiac tamponade. The main symptoms of pericardial effusions and cardiac tamponade include:
If a pericardial effusion is large enough, it can press on surrounding tissues or nerves. That can cause symptoms like:
In developed countries, an unknown reason is the most common cause of a pericardial effusion. Tuberculosis is the most common cause in developing countries.
Pericardial effusion has many different causes. It often happens along with (or because of) inflammation of the pericardium (pericarditis).
Possible causes of pericardial effusion include:
Advertisement
If you have symptoms, a provider will diagnose pericardial effusion based on the symptoms you describe, your medical history, medical testing and a physical exam.
If you don’t have symptoms, the most likely way a provider will diagnose pericardial effusion is if they happen to see it on medical images they ordered for another reason. For example, they may see it on a chest X-ray you get after a car accident.
If a healthcare provider suspects a pericardial effusion, they may order several different kinds of tests.
A provider may order an electrocardiogram (EKG) to check your heart’s electrical activity. They may order imaging tests like:
After a provider diagnoses pericardial effusion, they may order lab tests to find the cause of your condition. The possible tests include:
In some cases, your provider may be able to test the fluid they remove from your pericardium. These results can sometimes help them find the cause of the effusion.
Advertisement
The pericardial effusion treatment you get depends on how severe your condition is and what caused it.
If you have a small or medium-sized pericardial effusion that’s shrinking or not changing size, and you don’t have symptoms, you may not need any treatment. In these cases, your healthcare provider will probably want to monitor the effusion size and only treat it if you develop symptoms or if there are other signs that it might be a problem.
If you have an effusion that’s growing more quickly, that’s causing symptoms or that’s happening because of more serious conditions (especially trauma or cancer), you’ll probably need treatment sooner rather than later.
When a pericardial effusion is large or causes cardiac tamponade, it becomes a medical emergency that needs immediate treatment. Unlike smaller amounts, the pericardial fluid won’t go away unless you remove it. Potential treatments include:
Advertisement
In cases where an effusion isn’t dangerous and doesn’t need any of the above treatments, a provider can often manage it with medications or other types of treatments. The treatments depend on the underlying cause. These include, but aren’t limited to, the following:
The possible side effects with treatments for pericardial effusion depend strongly on which treatments or medications you receive. Your healthcare provider is the best person to tell you about what side effects can happen with the medications you take.
A possible complication is pericardial decompression syndrome when you undergo a procedure or surgery to treat a pericardial effusion. While it isn't common, it is severe and life-threatening. It usually happens when fluid removal happens too quickly from a large effusion. To avoid this, your healthcare provider may drain the effusion more slowly.
How long it takes you to feel better and recover depends on these main factors:
In cases where you have symptoms of cardiac tamponade, you should start to feel better as fluid removal lowers the pressure on your heart. In general, your healthcare provider is the best person to tell you the likely recovery time and when you should start to feel better.
Pericardial effusion is usually a significant condition. But it isn’t always a medical emergency. Whether or not it’s a life-threatening emergency depends on what caused it, the amount of fluid involved and how fast that fluid fills your pericardium.
When an effusion happens quickly, it needs less fluid to become dangerous and cause cardiac tamponade. That’s because your pericardium doesn’t have time to stretch and expand to fit more fluid inside it. When a pericardial effusion happens slowly, it can take weeks or even months before it becomes a problem.
One factor that determines if a pericardial effusion is serious is why it happened in the first place. When it happens because of injuries or heart and circulatory problems (or any reason that can cause an effusion to develop quickly), pericardial effusion needs quick treatment to avoid dangerous complications like cardiac tamponade.
Large effusions and effusions that grow quickly are serious conditions that need quick medical care. They shouldn’t last any longer than it takes to diagnose and treat them, especially in emergency cases.
Chronic effusions, especially smaller ones that don’t cause symptoms, can last for weeks, months or even years. Your healthcare provider may recommend regular follow-up visits to keep checking the size of the effusion and whether or not it poses any risks to your health.
Providers can often treat pericardial effusions. Sometimes, they can cure them, depending on how severe they are and why they happened.
Overall, effusions that happen for unknown reasons tend to have a good prognosis. Effusions that happen because of trauma or cancer are more likely to have complications and are usually harder to treat. Survival rates are poor for people whose pericardial effusions have a link to cancer or HIV/AIDS.
Pericardial effusion is unpredictable, so you usually can’t prevent it. But you can indirectly reduce your risk by avoiding circumstances that could cause it, like:
If you have a pericardial effusion, it’s important to watch for any symptoms or changes in your overall health. You should also follow your healthcare provider’s guidance, especially when it comes to taking medication and managing your recovery.
Your healthcare provider can schedule follow-up visits to monitor your condition, if necessary. They can also give you guidance on how to manage your symptoms and when you should call their office.
You should go to the hospital emergency room immediately if you have any of the following symptoms, which can be signs of cardiac tamponade:
You may want to ask your healthcare provider:
Pleural effusion is similar to pericardial effusion, but it happens in a different place inside your chest. The pleural cavity is the sac that surrounds your lungs, and pleural effusion is when fluid fills up that space. A pleural effusion keeps your lungs from expanding as they should, which makes it harder for you to breathe.
When it’s hard to breathe and your chest hurts, you just want relief. Maybe you don’t even know why you’re having pericardial effusion, a buildup of fluid in the sac around your heart. Whatever the reason for your pericardial effusion, you should feel better after treatment. Don’t hesitate to ask your provider about anything that isn’t clear to you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether your pericardial disease comes on acutely without warning or is chronic, Cleveland Clinic has the best treatments for this heart condition.
