A migraine is much more than a bad headache. It can cause debilitating, throbbing, one-sided head pain that can leave you in bed for days. Movement, lights, sounds and other triggers may cause symptoms like fatigue, nausea, vision changes, irritability and more. A healthcare provider can help you manage symptoms so migraines don’t take over your life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_hw1v2cz3/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn how each different phase can impact your life.
A migraine is a severe headache that causes throbbing, pulsing head pain on one side of your head. The headache phase of a migraine usually lasts at least four hours, but it can also last for days. This headache gets worse with:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Migraines are disruptive. They can interfere with your daily routine and affect your ability to meet personal and social obligations. Treatment is available to help you manage migraines.
There are several types of migraines. The most common migraine categories are:
An aura is a phase of the migraine before head pain begins.
Other types of migraines include:
Migraines are common. Studies show that an estimated 12% of people in the United States experience migraines.
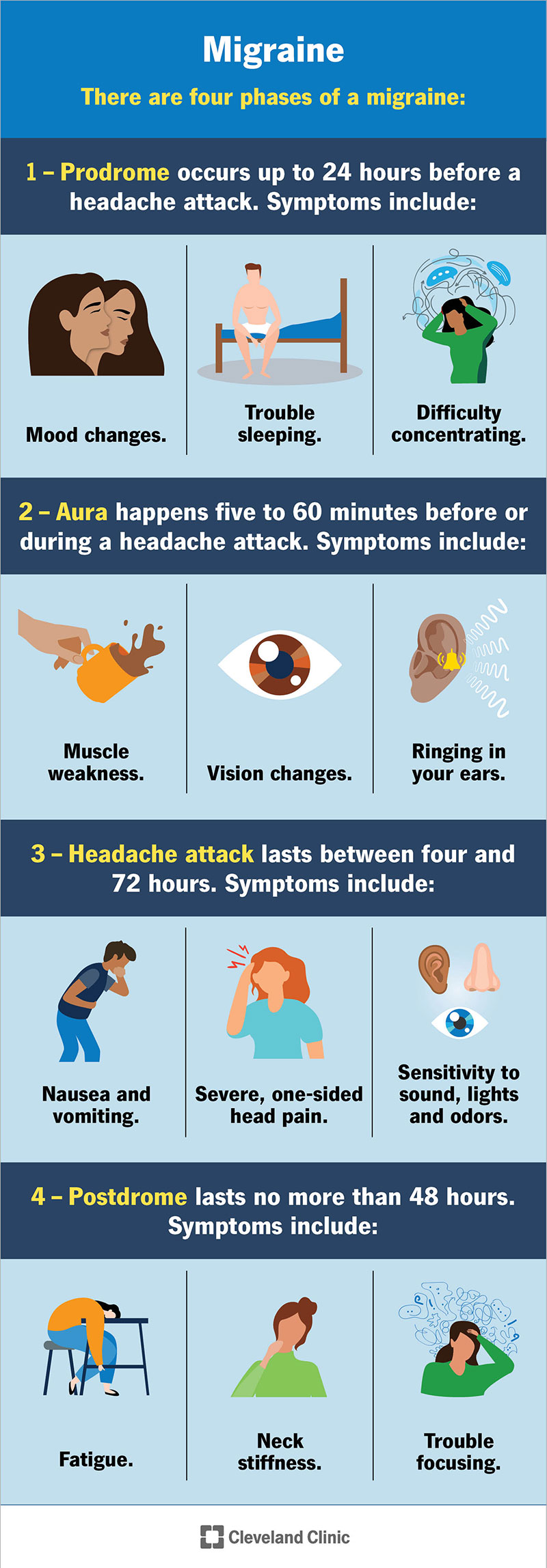
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/5005-migraine-headache)
There are four phases or stages of a migraine:
Advertisement
It can take about eight to 72 hours to go through the four stages.
Migraine symptoms vary based on the stage. Every migraine is different, and you won’t necessarily experience symptoms during all four stages of every migraine.
Head pain gradually gets more intense. It can affect one side of your head or both. It can occur with other symptoms like:
Migraine headache pain may feel like the following:
A migraine can feel different for each person. A migraine headache ranges from mild to severe. Head pain can start on one side and shift to the opposite side. You may also have pain around your eyes or temple, and sometimes, around your face, sinuses, jaw or neck.
The frequency of a migraine varies from person to person. You might have one migraine per year or one per week. On average, most people experience two to four per month. They’re most common in the morning. Most migraines are unpredictable, but sometimes, you can have an idea of when a migraine will happen, like before menstruation or after feeling stress.
Researchers aren’t sure of the exact cause of migraines, but studies show genetics play a role.
When you have a headache, specific nerves in your blood vessels send pain signals to your brain. This releases inflammatory substances into your head’s nerves and blood vessels. It’s unclear why your nerves do that.
A trigger is something that causes symptoms to start. Some of the most common migraine triggers include:
Your healthcare provider can help you identify your triggers. They might recommend keeping a migraine journal to track similarities between migraine attacks.
What foods trigger migraines?
Your body may have a sensitivity to specific chemicals and preservatives in foods. This sensitivity makes a migraine more likely to happen, especially if combined with other triggers.
Some of the most common food triggers include:
Advertisement
Yes, migraines tend to run in biological families. Up to 80% of people with migraines have a first-degree biological relative with the condition.
A migraine can affect anyone at any age, from children to adults. Women are more likely than men to experience a migraine.
Other risk factors that may make you more likely to experience a migraine include:
A healthcare provider will diagnose a migraine after a physical exam and neurological exam. They’ll also learn more about your medical history and biological family health history. Your provider may ask you questions to learn more about your symptoms, including:
Your provider may also order blood tests and imaging tests (such as a CT scan or an MRI) to make sure there aren’t any other causes for your headache. An electroencephalogram (EEG) may help your provider rule out other conditions.
Advertisement
If you think you have a migraine, discuss your symptoms with a primary care physician (PCP) first. They can diagnose migraine headaches and start treatment. Your PCP may refer you to a headache specialist or a neurologist.
There isn’t a cure for migraines. But a healthcare provider can help you manage migraine symptoms through the following:
A healthcare provider might recommend taking medications to treat migraines. There are two types of medications available:
Common medications that stop migraines include:
Advertisement
Common preventive migraine medications include:
Medications come in different forms, like:
You and your healthcare provider will discuss the specific medication, combination of medications and formulations to best manage your symptoms. All medications should be used under the direction of a headache specialist or provider. As with any medication, it’s important to carefully follow your provider’s instructions.
Over-the-counter migraine medications
Over-the-counter migraine medications are effective if you have mild to moderate migraine symptoms. The main ingredients in pain-relieving medications are ibuprofen, aspirin, acetaminophen, naproxen and caffeine.
Be cautious when taking over-the-counter pain relievers. Sometimes, overusing them can cause analgesic-rebound headaches or a dependency problem. If you’re taking any over-the-counter pain medications more than two to three times a week, let your healthcare provider know. They may suggest more effective prescription medications.
A healthcare provider can help you identify what triggers your migraines. They may ask you to keep a migraine journal or diary. A migraine journal can help you keep track of when a migraine happened, how you felt and how long it lasted. You can also add details about the foods you ate or the activities you participated in to learn more about any possible triggers.
There are some smartphone apps available to help you keep a migraine journal.
Once you identify a trigger, you can take steps to avoid it. This isn’t always possible, but awareness of your triggers is helpful to identify them and treat a migraine when it starts.
For example, if stress is a trigger, you may want to speak with a mental health professional to help you manage your stress. If you get migraine symptoms when you miss a meal, set an alarm on your phone to remind you to eat meals on a regular schedule.
You may want to try alternative therapies to help you manage migraines. These include:
Talk to your healthcare provider before starting any alternative therapies for migraines.
Talk to your healthcare provider if you’re pregnant or plan on becoming pregnant and experience migraines. Your provider might suggest avoiding medications for migraines when you’re pregnant or if you think you may be pregnant. Some medications can negatively affect the fetus’s development.
Your provider can recommend alternative treatment options like an acetaminophen pain reliever for migraines.
There are certain things you can do to help you feel better when a migraine attack happens, including:
Migraines are different for each person. They’re temporary but recurring throughout your life. There’s also no available cure. Your healthcare provider can help you manage migraines so they go away faster and are less intense. It may take time to find a treatment option that’s right for you. Let your healthcare provider know if your symptoms improve or get worse.
You can’t prevent all migraines. But you can take preventive migraine medications as directed by your healthcare provider to reduce how often and how severe migraine symptoms affect you. You can also learn more about your triggers and work with your healthcare provider to avoid them.
Schedule a visit with your healthcare provider if you experience:
Call 911 (or your local emergency services number) or go to an emergency department right away if you:
You’ve probably had a headache before, but a migraine is different. It can feel like the world is ending and there’s nothing you can do to make it go away. Even though your symptoms are temporary, the duration of a migraine can make it feel like time is moving slower and against you. But there are treatment options available to manage migraines as they happen and prevent them from interfering with your day. A healthcare provider can help you with this, so migraines don’t take over your life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Do you have headaches that won’t go away? Or ones that come back regularly? Cleveland Clinic’s headache and migraine experts are here to help.
