Lung cancer is the third most common cancer in the U.S. It’s caused by harmful cells in your lungs growing unchecked. Treatments include surgery, chemotherapy, immunotherapy, radiation and targeted drugs. Screening is recommended if you’re at high risk. Advances in treatments have caused a significant decline in lung cancer deaths in recent years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
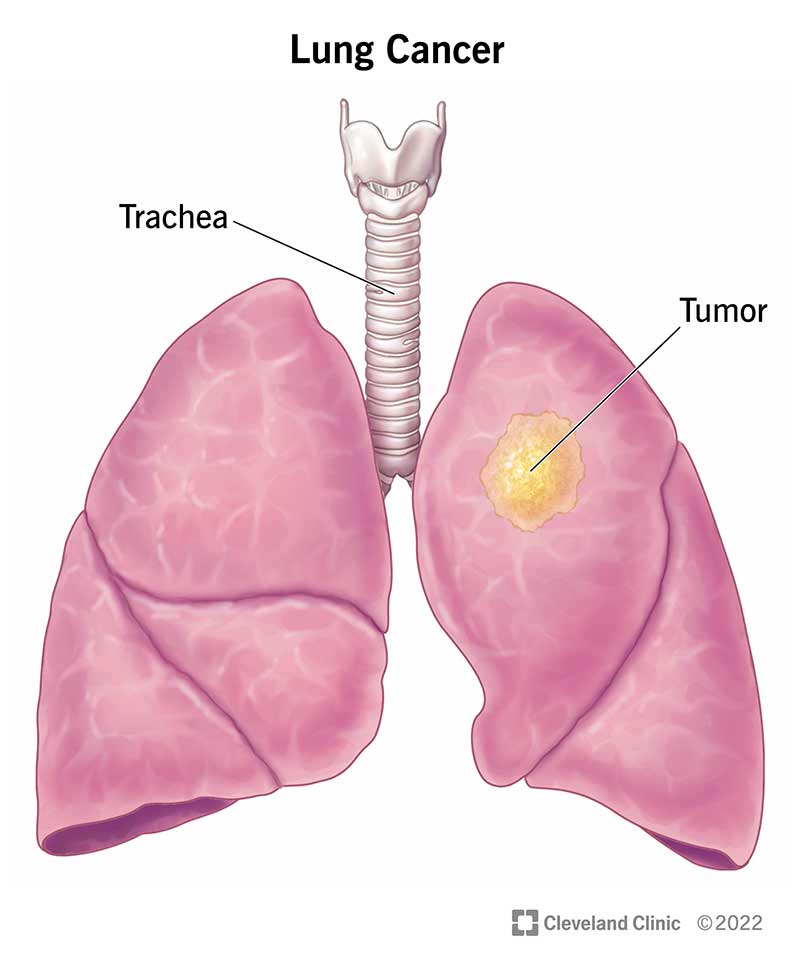
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4375-lung-cancer)
Lung cancer is a disease caused by uncontrolled cell division in your lungs. Your cells divide and make more copies of themselves as a part of their normal function. But sometimes, they get changes (mutations) that cause them to keep making more of themselves when they shouldn’t. Damaged cells dividing uncontrollably create masses, or tumors, of tissue that eventually keep your organs from working properly.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lung cancer is the name for cancers that start in your lungs — usually in the airways (bronchi or bronchioles) or small air sacs (alveoli). Cancers that start in other places and move to your lungs are usually named for where they start (your healthcare provider may refer to this as cancer that’s metastatic to your lungs).
There are many cancers that affect the lungs, but we usually use the term “lung cancer” for two main kinds: non-small cell lung cancer and small cell lung cancer.
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer. It accounts for over 80% of lung cancer cases. Common types include adenocarcinoma and squamous cell carcinoma. Adenosquamous carcinoma and sarcomatoid carcinoma are two less common types of NSCLC.
Small cell lung cancer (SCLC) grows more quickly and is harder to treat than NSCLC. It’s often found as a relatively small lung tumor that’s already spread to other parts of your body. Specific types of SCLC include small cell carcinoma (also called oat cell carcinoma) and combined small cell carcinoma.
Other types of cancer can start in or around your lungs, including lymphomas (cancer in your lymph nodes), sarcomas (cancer in your bones or soft tissue) and pleural mesothelioma (cancer in the lining of your lungs). These are treated differently and usually aren’t referred to as lung cancer.
Advertisement
Cancer is usually staged based on the size of the initial tumor, how far or deep into the surrounding tissue it goes, and whether it’s spread to lymph nodes or other organs. Each type of cancer has its own guidelines for staging.
Each stage has several combinations of size and spread that can fall into that category. For instance, the primary tumor in a Stage III cancer could be smaller than in a Stage II cancer, but other factors put it at a more advanced stage. The general staging for lung cancer is:
While providers now use stages I through IV for small cell lung cancer, you might also hear it described as limited or extensive stage. This is based on whether the area can be treated with a single radiation field.
Metastatic lung cancer is cancer that starts in one lung but spreads to the other lung or to other organs. Metastatic lung cancer is harder to treat than cancer that hasn’t spread outside of its original location.
Lung cancer is the third most common cancer in the U.S. Health systems report over 200,000 new cases of lung cancer each year.
Most lung cancer symptoms look similar to other, less serious illnesses. Many people don’t have symptoms until the disease is advanced, but some people have symptoms in the early stages. For those who do experience symptoms, it may only be one or a few of these:
Advertisement
A cough or pneumonia that keeps coming back after treatment can sometimes be an early sign of lung cancer (though it can also be a sign of less serious conditions). The most common signs of lung cancer include a persistent or worsening cough, shortness of breath, chest pain, hoarseness or unexplained weight loss.
Depending on where in your lungs cancer starts, some of these symptoms can happen early (in stages I or II) but often they don’t happen until cancer has progressed to later stages. That’s why it’s important to get screened for lung cancer if you’re at higher risk.
Cancer can grow in your body for a long time — years — before you know it’s there. Lung cancer often doesn’t cause symptoms in early stages.
Lung cancer is caused by cells that keep dividing even though they shouldn’t. While cell division is a normal process, all cells have a built-in off switch that keeps them from dividing into more cells (senescence) or causes them to die off (apoptosis) when necessary. The off switch is triggered when a cell has divided too many times or has too many changes (mutations).
Cancer cells are normal cells in your body that have gained mutations that remove the off switch. Cells keep multiplying, unchecked, and interfere with your normal cells. Cancer cells can get into your bloodstream or lymph nodes and move to other places in your body, spreading the damage.
Advertisement
We’re not sure what causes these changes that lead to cancer in some people and not others, but certain factors, including smoking tobacco products, can put you at higher risk for damage to your cells that can cause lung cancer.
While there are many factors that can increase your risk of lung cancer, smoking any kind of tobacco products, including cigarettes, cigars or pipes is the biggest single risk factor. Experts estimate that 80% of lung cancer deaths are smoking-related.
Other risk factors include:
You can inhale a number of substances when you vape (use a device to inhale a mist of nicotine and flavoring), including some that are known to cause cancer. Vaping is too new to know all of its long-term effects, but experts believe that it has the potential to cause lung damage.
While smoking is the leading risk factor for lung cancer, up to 20% of people diagnosed have never smoked. That’s why it’s important to talk to your provider about any concerning symptoms.
Advertisement
Diagnosing lung cancer can be a multi-step process. Your first visit to a healthcare provider will usually involve them listening to your symptoms, asking you about your health history and performing a physical exam (like listening to your heart and lungs). Since lung cancer symptoms are similar to many other, more common illnesses, you provider may start by getting blood tests and a chest X-ray.
If your provider suspects you could have lung cancer, your next steps in diagnosis would usually involve more imaging tests, like a CT scan, and then a biopsy. Other tests include using a PET/CT scan to see if cancer has spread, and tests of cancerous tissue from a biopsy to help determine the best kind of treatment.
X-rays aren’t as good as CT scans for showing a tumor in your lungs, especially at earlier stages. Tumors might be too small to see on an X-ray or can be blocked from view by other structures in your body (like your ribs). X-rays can’t diagnose lung cancer — they can only show your provider if there’s something suspicious that they should look into further.
Tests your healthcare provider might order or perform include blood tests, imaging, and biopsies of fluid or tissue.
Blood tests can’t diagnose cancer on their own, but can help your provider check how your organs and other parts of your body are working.
Chest X-rays and CT scans give your provider images that can show changes in your lungs. PET/CT scans are usually done to evaluate a concerning finding on a CT scan or after a cancer diagnosis to determine whether cancer has spread.
There are a number of procedures your provider can use to look more closely at what’s going on inside your chest. During the same procedures, your provider can take samples of tissue or fluid (biopsy), which can be studied under a microscope to look for cancer cells and determine what kind of cancer it is. Samples can also be tested for genetic changes (mutations) that might affect your treatment.
Procedures used to initially diagnose lung cancer or learn more about its spread include:
As part of a biopsy, your provider might have your tissue sample tested for gene changes (mutations) that special drugs can target as part of your treatment plan. Genes that might have changes that can be targeted in NSCLC include:
Treatments for lung cancer are designed to get rid of cancer in your body or slow down its growth. Treatments can remove cancerous cells, help to destroy them or keep them from multiplying or teach your immune system to fight them. Some therapies are also used to reduce symptoms and relieve pain. Your treatment will depend on the type of lung cancer you have, where it is, how far it’s spread and many other factors.
Lung cancer treatments include surgery, radiofrequency ablation, radiation therapy, chemotherapy, targeted drug therapy and immunotherapy.
NSCLC that hasn’t spread and SCLC that’s limited to a single tumor can be eligible for surgery. Your surgeon might remove the tumor and a small amount of healthy tissue around it to make sure they don’t leave any cancer cells behind. Sometimes they have to remove all or part of your lung (resection) for the best chance that the cancer won’t come back.
NSCLC tumors near the outer edges of your lungs are sometimes treated with radiofrequency ablation (RFA). RFA uses high-energy radio waves to heat and destroy cancer cells.
Radiation uses high energy beams to kill cancer cells. It can be used by itself or to help make surgery more effective. Radiation can also be used as palliative care, to shrink tumors and relieve pain. It’s used in both NSCLC and SCLC.
Chemotherapy is often a combination of multiple medications designed to stop cancer cells from growing. It can be given before or after surgery or in combination with other types of medication, like immunotherapy. Chemotherapy for lung cancer is usually given through an IV.
In some people with NSCLC, lung cancer cells have specific changes (mutations) that help the cancer grow. Special drugs target these mutations to try to slow down or destroy cancer cells. Other drugs, called angiogenesis inhibitors, can keep the tumor from creating new blood vessels, which the cancer cells need to grow.
Our bodies usually recognize cells that are damaged or harmful and destroy them. Cancer has ways to hide from the immune system to keep from being destroyed. Immunotherapy reveals cancer cells to your immune system so your own body can fight cancer.
Some lung cancer treatments are used to relieve symptoms, like pain and difficulty breathing. These include therapies to reduce or remove tumors that are blocking airways, and procedures to remove fluid from around your lungs and keep it from coming back.
Side effects of lung cancer treatment depend on the type of treatment. Your provider can tell you what side effects to expect, and what complications to look out for, for your specific treatment.
Chemotherapy
Immunotherapy
Radiation therapy
Surgery
Your provider can prescribe medications to help manage your symptoms or side effects of treatment. A palliative care specialist or a dietitian can help you manage pain or other symptoms and improve your quality of life while you’re in treatment.
What to expect after a lung cancer diagnosis depends on many factors. For some with early stage cancer, your provider will remove the cancer and you’ll need follow up screenings for several years. For many others, it’s a process that evolves over time. It may mean doing one type of treatment until it stops being effective, then moving on to another type.
How fast lung cancer spreads depends on the type. Of the main types, small cell lung cancer tends to spread faster than non-small cell lung cancer. By the time lung cancer is found, it may have already started spreading to lymph nodes or other organs.
Some types of lung cancer can be considered cured if diagnosed before they spread, though experts don’t often use the word “cured” to describe cancer. More common terms are “remission” or “no evidence of disease” (NED). If you’re in remission or NED for five years or more, you might be considered cured. There’s always a small chance that cancer cells could come back.
The survival rate of lung cancer depends greatly on how far cancer has spread when it’s diagnosed, how it responds to treatment, your overall health and other factors. For instance, for small tumors that haven’t spread to the lymph nodes, the survival rates are 90% for tumors that are smaller than 1 cm, 85% for tumors between 1 and 2 cm, and 80% for tumors between 2 and 3 cm.
The relative five-year survival rate for lung cancer diagnosed at any stage is 22.9%. The five-year relative survival rates by how much cancer has spread is:
Remember that these numbers don’t take into account the specific details of your diagnosis and treatment. Thanks to improvements in detection and treatment, the rates of lung cancer deaths have been rapidly coming down in recent years.
Your healthcare provider may share five-year survival rates as a way of explaining how your lung cancer may affect your health five years after diagnosis. These numbers compare the survival rate of someone with lung cancer to someone of the same age in the general population.
Since we don’t know what causes most cancers for sure, the only preventative measures are focused on reducing your risk. Some ways to reduce your risk include:
You can increase your chances of catching cancer in its earliest stages with screening tests. You’re eligible for lung cancer screening if you meet all of these requirements:
Ask your provider about the benefits and risks of yearly screening.
Self-care is an important part of cancer care. Some ways you can take care of yourself while receiving or recovering from treatment include:
If you’ve completed treatments, support and self-care can still play an important part in moving forward. Don’t hesitate to reach out for help or guidance. Make sure you follow up with your provider as recommended.
Check in with your provider if you have any symptoms that concern you. If you smoke or used to smoke, ask your provider about screening for lung cancer.
A lung cancer diagnosis can bring with it a flood of different emotions. Sometimes the volume of new information can be overwhelming. An important thing to remember is that statistics can’t tell you how your treatment will go or what decisions are right for your specific situation.
Enlisting the help of trusted loved ones or a support group can help you consider your options and voice your preferences. Cancer treatment is often a process, and taking care of yourself is one of its most important parts.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have lung cancer, you might feel alone and afraid. You don’t have to be. Cleveland Clinic is here to help find and treat your cancer at any stage.
