Horner syndrome is a rare neurological syndrome that affects your eye and the surrounding area on one side of your face. It’s a sign of underlying nerve damage and has several possible causes ranging from carotid artery dissection to apical lung tumor. Seek medical care if you develop Horner syndrome.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
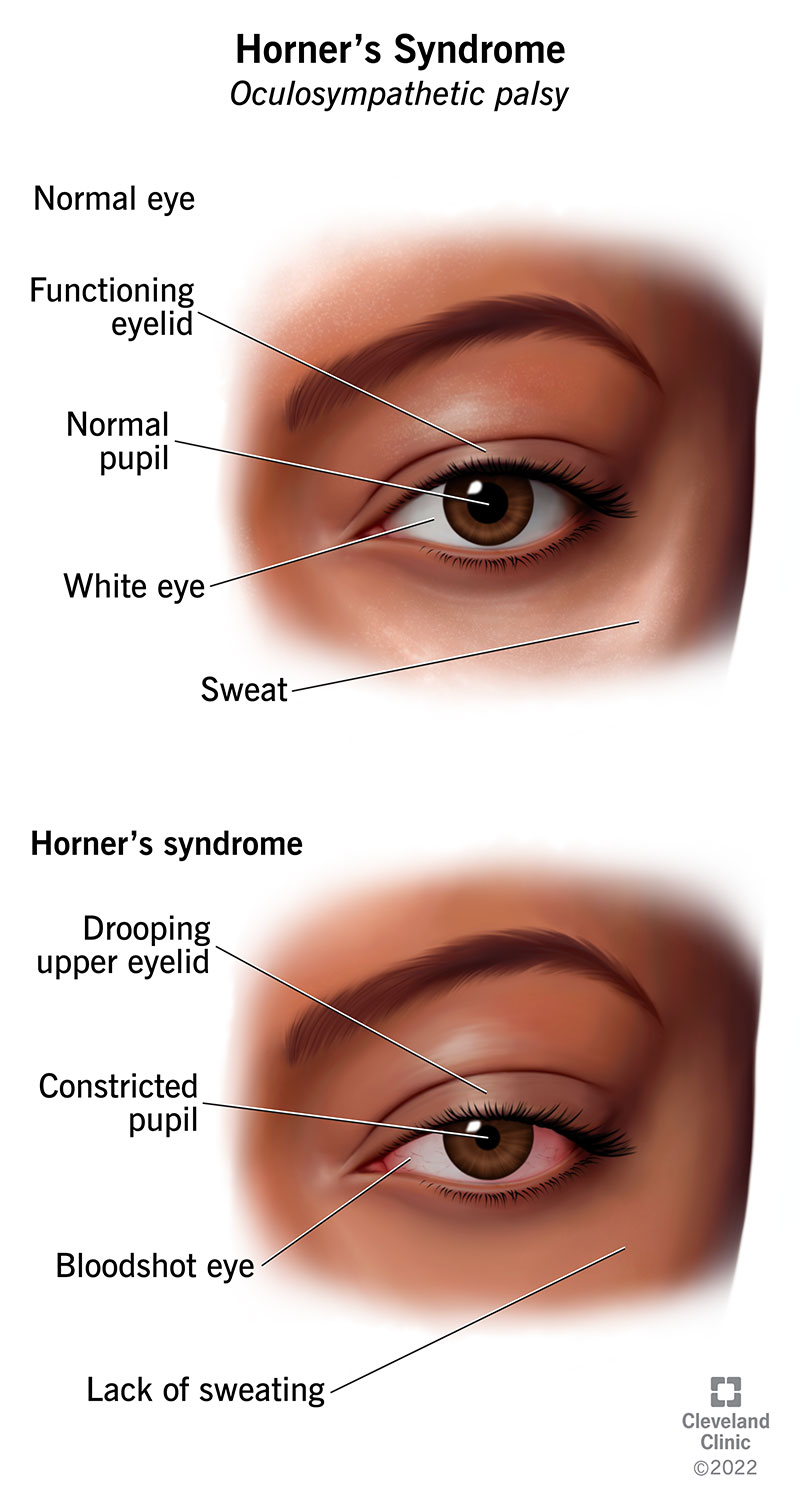
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17836-horners-syndrome)
Horner syndrome, also known as oculosympathetic palsy or Bernard-Horner syndrome, is a relatively rare neurological syndrome that affects your eye and the surrounding tissues on one side of your face.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It occurs due to a disruption of the pathway of the sympathetic nerves that connect your brainstem to your eyes and face. These nerves control involuntary functions, such as sweating (perspiration) and the dilation and constriction of the pupils of your eyes.
The symptoms associated with Horner syndrome generally don’t cause significant issues with your health or vision. However, they can indicate the presence of an underlying health problem that may be very serious. It’s important to seek medical care if you develop symptoms of Horner syndrome to determine the underlying cause.
Horner syndrome can affect anyone at any age. About 5% of people with the condition have the congenital form (present from birth).
Horner syndrome is uncommon. It affects approximately 1 in 6,000 people.
Usually, symptoms of Horner syndrome affect only one side of your face. They include:
Most often, Horner syndrome happens as a result of blockage or damage to the sympathetic nerves that lead to your eyes. The underlying causes of nerve damage can vary widely, from a middle ear infection to a carotid artery dissection or apical chest tumor.
Advertisement
In rare cases, Horner syndrome is a congenital condition, meaning it’s present at birth. Usually, the congenital form occurs because of some type of birth trauma or injury to the nerves or carotid artery during delivery. In even rarer cases, the syndrome may be inherited, although no specific genes have been linked to it yet.
Three different nerve pathways may be involved in Horner syndrome. The nerves from your brain don’t travel along a direct path to your eyes and face. They travel along three paths, and disruption can occur in any of these pathways. Because of this, there are three types of Horner syndrome with different possible causes.
Some people with the syndrome don’t have a known underlying condition that would lead to it. These cases are referred to as idiopathic Horner syndrome.
First-order (central) Horner syndrome results from damage to the nerves that go from your hypothalamus and lead down through your brainstem and spinal cord. Damage or obstruction of this nerve pathway may occur due to:
Second-order Horner syndrome results from damage to the nerve pathway that leads from your chest to the top of your lungs and along the carotid artery in your neck. Conditions that can damage or obstruct this nerve pathway include:
Third-order Horner syndrome results from damage to the nerve path that travels from your neck to your middle ear and eye. Problems may result from:
Healthcare providers usually diagnose Horner syndrome with a physical exam. Determining the underlying cause may be complex, as it can occur due to many medical conditions. In addition, other conditions can cause similar symptoms.
A healthcare provider will ask detailed questions about your symptoms and medical history. They’ll ask about past injuries, illnesses and surgeries. They’ll also perform a physical exam.
Advertisement
Based on your medical history and any other symptoms you have, a provider may order additional tests to determine the cause of Horner syndrome, including:
The treatment for Horner syndrome involves treating the underlying cause. As there are many possible causes, the kinds of treatment can vary widely.
Sometimes, no treatment is necessary unless you’re experiencing pain or other discomforts.
The prognosis (outlook) of Horner syndrome depends on the underlying cause. The characteristic symptoms of Horner syndrome generally don’t have a significant impact on your quality of life or vision.
If the underlying cause is a chronic (long-lasting) condition, such as multiple sclerosis, Horner syndrome may also be chronic. If it results from something temporary and treatable, such as an ear infection, it’ll likely go away once the infection is treated.
As so many underlying conditions can potentially cause Horner syndrome, there’s no way to prevent it from developing.
However, in cases of Horner syndrome related to trauma (such as carotid artery dissection), taking safety measures to avoid injuring your neck and following dissection precautions can help you avoid developing the syndrome.
Advertisement
If you have symptoms of Horner syndrome, such as one drooping upper eyelid, mismatched pupil sizes and lack of sweating on the same side of your face, see a healthcare provider as soon as possible.
Horner syndrome is a rare sign of underlying nerve damage. While the symptoms of the syndrome often don’t cause harm, the underlying cause may be life-threatening, such as a tumor or carotid artery dissection. Because of this, it’s crucial to see a healthcare provider if you develop the syndrome so they can determine the underlying cause and treat it immediately.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
