Leukemia starts when the DNA of a single cell in your bone marrow changes (mutates) and can’t develop and function normally. Leukemia cells often behave like abnormal white blood cells. Treatments for leukemia depend on the type of leukemia you have, your age and overall health, and if the leukemia has spread to other organs or tissues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
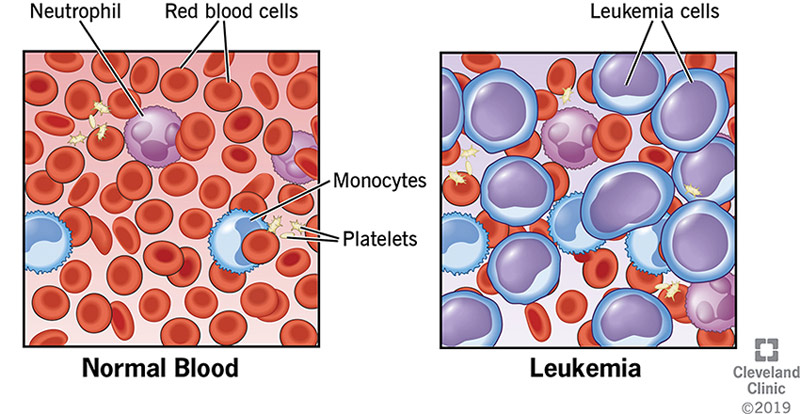
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4365-leukemia)
Leukemia is a cancer of the blood, characterized by the rapid growth of abnormal blood cells. This uncontrolled growth takes place in your bone marrow, where most of your body’s blood is made. Leukemia cells are usually immature (still developing) white blood cells. The term leukemia comes from the Greek words for “white” (leukos) and “blood” (haima).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Unlike other cancers, leukemia doesn’t generally form a mass (tumor) that shows up in imaging tests, such as X-rays or CT scans.
There are many types of leukemia. Some are more common in children, while others are more common in adults. Treatment depends on the type of leukemia and other factors.
Leukemia begins in bone marrow, the soft spongy tissue in the inner cavity of your bones, where your body’s blood cells are made. Blood cells go through multiple stages before reaching their fully mature forms. Mature, normal blood cells include:
These blood cells start as hematopoietic (hemo = blood, poiesis = make) stem cells. The stem cells develop into either myeloid (MAI-uh-loyd) cells or lymphoid (LIM-foyd) cells. If blood cells were to continue to develop normally, the mature forms of these cells are as follows:
Advertisement
However, if you have leukemia, one of the developing blood cells begins to multiply out of control. These abnormal cells — called leukemia cells — begin to take over the space inside of your bone marrow. They crowd out the cells trying to develop into healthy red blood cells, white blood cells and platelets.
Having too many leukemia cells and too few normal cells is harmful for several reasons:
There are four main types of leukemia and several subtypes. Healthcare providers classify leukemia based on how fast the disease worsens and whether leukemia cells arise from myeloid cells or lymphoid cells.
Healthcare providers classify leukemia based on how quickly it progresses and the type of blood cell involved.
By speed of disease progression
By cell type
There are four main types of leukemia:
Advertisement
Leukemia is the 10th most common cancer in the U.S., accounting for 3.2% of all new cancer cases. Leukemia can affect anyone, but it’s more common among people who are:
Many people think of leukemia as a pediatric cancer, but some forms develop more often in adults. Although leukemia is rare in children, it’s the most common form of cancer affecting children and teens.
Symptoms depend, in part, on the type of leukemia. For instance, if you have a chronic form of leukemia, you may not have noticeable symptoms in the early stages.
Common signs and symptoms of leukemia include:
Leukemia starts when the DNA of a single cell in your bone marrow changes (mutates). DNA is the “instruction code” that tells a cell when to grow, how to develop and when to die. Because of the mutation, or coding error, leukemia cells keep multiplying. All cells arising from the original mutated cell also have the mutated DNA.
Advertisement
Scientists don’t know what causes these developing cells to mutate. They’ve been able to identify some common mutations that people diagnosed with different types of leukemia share.
Anyone can develop leukemia. Still, studies have shown that certain factors may increase your risk, including:
Advertisement
Results from routine blood work can alert your healthcare provider that you may have an acute or chronic form of leukemia that requires further testing. Or they may recommend a workup if you have leukemia symptoms.
Diagnostic exams and tests may include:
Treatments for leukemia depend on the type of leukemia you have, your age and overall health, and if the leukemia has spread to other organs or tissues.
Common treatments often include a combination of the following:
Clinical trials are also available to test new cancer treatments. Weigh the potential benefits and risks of enrolling in a clinical trial with your healthcare provider.
Depending on your treatment plan, you may receive ongoing leukemia treatments long-term or treatment in phases. Generally, phased treatment involves three parts. Each phase has a specific goal.
Your healthcare provider may resume or change your treatment if the leukemia returns.
It’s difficult to predict the prognosis for leukemia because everyone’s experience is different. Outcomes depend on a variety of factors, including:
Ultimately, your healthcare provider is the most reliable resource for understanding how your cancer affects your unique prognosis. Ask them about treatment outcomes.
Although the number of new cases of leukemia in the U.S. has remained relatively steady or slightly increased since the 1970s, the survival rate has also improved. Still, long-term outcomes vary for each person.
The National Cancer Institute reports the following survival data for the four main types of leukemia:
| Types of Leukemia | ALL | AML | CLL | CML |
|---|---|---|---|---|
| 5- year survival rate* | 69.9% | 29.5% | 87.2% | 70.6% |
| Number of deaths per 100,000 persons | 0.4 | 2.7 | 1.1 | 0.3 |
| Death is highest among those aged | 65-84 | 65+ | 75+ | 75+ |
| Types of Leukemia | ||||
| 5- year survival rate* | ||||
| ALL | ||||
| 69.9% | ||||
| AML | ||||
| 29.5% | ||||
| CLL | ||||
| 87.2% | ||||
| CML | ||||
| 70.6% | ||||
| Number of deaths per 100,000 persons | ||||
| ALL | ||||
| 0.4 | ||||
| AML | ||||
| 2.7 | ||||
| CLL | ||||
| 1.1 | ||||
| CML | ||||
| 0.3 | ||||
| Death is highest among those aged | ||||
| ALL | ||||
| 65-84 | ||||
| AML | ||||
| 65+ | ||||
| CLL | ||||
| 75+ | ||||
| CML | ||||
| 75+ |
Table legend:
ALL = acute lymphocytic leukemia; AML = acute myelogenous leukemia; CLL = chronic lymphocytic leukemia; CML = chronic myelogenous leukemia
*survival compares patients diagnosed with cancer vs. people of same age, race and sex who are cancer free.
Data source: SEER Cancer Statistics Review, 1975-2017, National Cancer Institute. Bethesda, MD.
There isn’t a cure for leukemia, but this doesn’t mean some people don’t achieve long-term remission. Being cured of leukemia means that the cancer’s gone, it’s not coming back and no more treatment is needed — but this is hard to know for sure with leukemia.
On the other hand, long-term remission means there’s no sign of cancer with or without treatment. Remission may last anywhere from a few weeks to many years. The leukemia may never return. If it does, your healthcare provider may recommend new treatments to achieve remission.
Your healthcare team can best answer the question, “Am I cured of my leukemia?” Your team will work closely with you to monitor your health and develop a personalized treatment plan.
Empower yourself by learning all you can about how your cancer diagnosis may uniquely impact you. It’s a good idea to take notes and bring a friend to your appointments. Don’t be afraid to ask questions.
Questions may include:
To learn more about clinical trials for leukemia, visit:
To connect with people with leukemia or to locate additional support from people who understand what it means to live with a cancer diagnosis, visit your local Leukemia & Lymphoma Society chapter.
Any cancer diagnosis is scary, but a leukemia diagnosis may feel especially so. It can be difficult to imagine what the treatment experience will be like without a tumor that can be removed. It can be intimidating to imagine the prognosis. Remember that leukemia isn’t one thing with one outcome. Your treatment and your chance of long-term remission depend on many factors. No one can predict your outcomes without understanding your health and leukemia — down to the characteristics of the leukemia cells. Talk with your healthcare provider about what a leukemia diagnosis means for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A leukemia diagnosis can come as quite a shock. Cleveland Clinic’s blood cancer experts are here to guide you through it and help you move forward.
