Thyrotoxicosis is a treatable condition that happens when you have too much thyroid hormone in your body. Common symptoms include unexplained weight loss, a rapid heart rate and shakiness. The treatment for thyrotoxicosis depends on what’s causing it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Thyrotoxicosis happens when you have too much thyroid hormone in your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Thyroid hormone is the hormone that controls your body’s metabolism — the process in which your body transforms the food you eat into energy. With thyrotoxicosis, your metabolism becomes too fast, causing symptoms that can affect your entire body. You may feel like your body’s in overdrive or that you don’t have control over it.
An overactive thyroid gland (hyperthyroidism) is the most common cause of thyrotoxicosis. But there are other ways you can have too much thyroid hormone in your body.
Despite having the word “toxic” in its name, only severe cases of thyrotoxicosis are life-threatening. This is called thyroid storm (thyroid crisis), and it’s rare. A sudden event or illness (like surgery or an infection) is the most common trigger of thyroid storm. It can also happen if you’re on anti-thyroid medication and suddenly stop taking it.
It’s still important to get treatment for mild to moderate thyrotoxicosis, though. Untreated or undertreated thyrotoxicosis can lead to certain health issues.
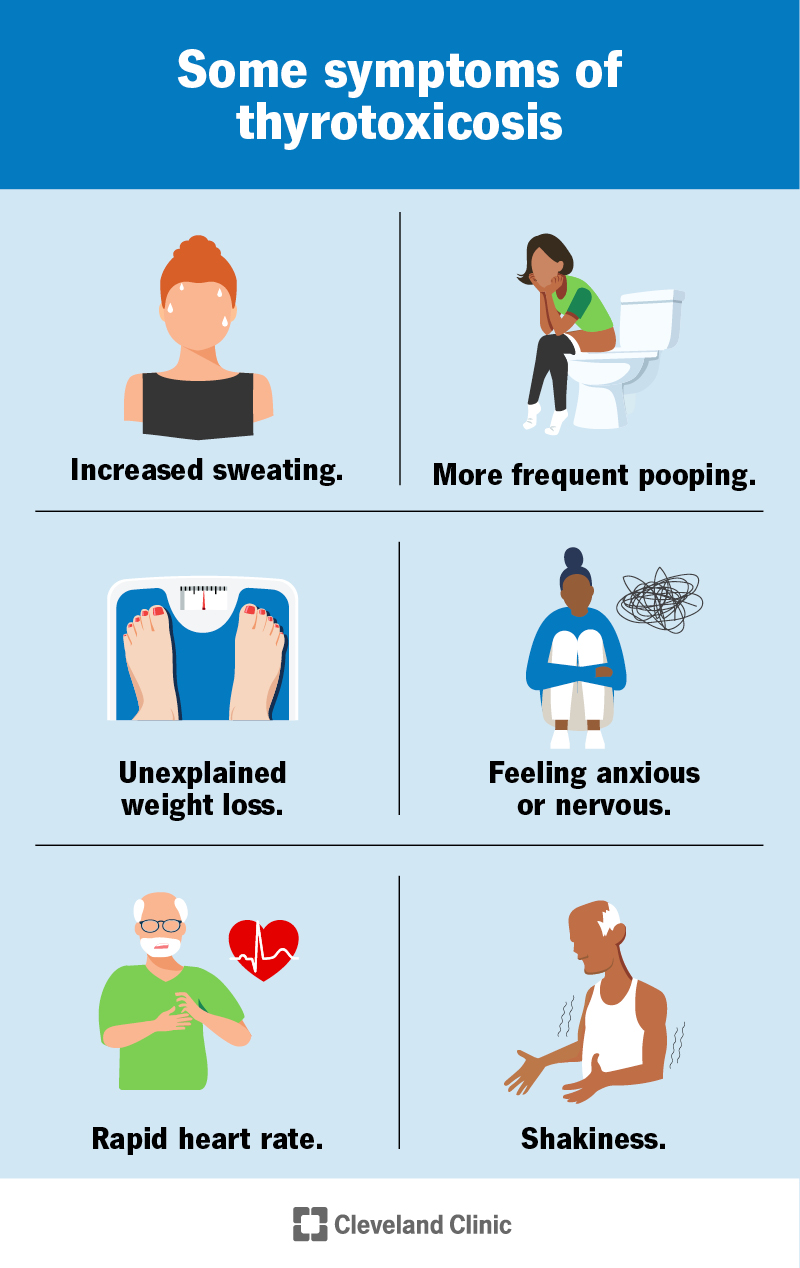
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21741-thyrotoxicosis)
Symptoms of thyrotoxicosis are generally the same in mild and moderate cases. But they’re more intense the more severe the thyrotoxicosis is.
Signs and symptoms of mild and moderate thyrotoxicosis include:
Advertisement
It’s important to see your healthcare provider if you have these symptoms.
A severe case of thyrotoxicosis is a thyroid storm, or thyroid crisis. It’s rare. But it’s life-threatening and requires immediate medical attention.
Symptoms of thyroid storm are more intense. For example, your heart rate may be over 140 beats per minute, and you may feel very agitated and confused. You may also have a high fever and even lose consciousness.
Many conditions and situations can cause thyrotoxicosis, including:
Each cause of thyrotoxicosis has certain risk factors. In general, risk factors for thyrotoxicosis include:
Having access to thyroid medication (levothyroxine) can also be a risk factor for thyrotoxicosis. Someone in your household may accidentally consume it or someone with factitious disorder may take it intentionally.
Healthcare providers diagnose thyrotoxicosis if blood tests show that you have elevated thyroid hormone levels and low or undetectable levels of thyroid-stimulating hormone (TSH).
If you have thyrotoxicosis, your provider will also need to figure out what’s causing it, which could lead to another diagnosis. The following tests and assessments can lead to a diagnosis:
Advertisement
The treatment for thyrotoxicosis depends on the underlying cause. Your healthcare provider will need to find the cause to recommend the best treatment for you.
Treatment may include:
If outside sources of thyroid hormone are causing thyrotoxicosis — like medications or contaminated beef — thyrotoxicosis should go away once the excess hormones have cleared your system. Your provider may have you do follow-up blood tests to make sure your thyroid hormone levels have returned to a healthy range.
Advertisement
You need treatment for thyroid storm (severe thyrotoxicosis) in a hospital.
The prognosis (outlook) for people with thyrotoxicosis is generally good if they receive treatment for it. There are several effective forms of treatment for thyrotoxicosis. Just like all treatments, they each have advantages and disadvantages. Together, you and your healthcare provider will determine the best plan for you.
Complications from untreated or undertreated thyrotoxicosis include:
These complications most commonly affect people who have untreated hyperthyroidism, especially Graves’ disease.
Thyroid storm can lead to serious complications if you receive delayed or no treatment, including seizures, cardiovascular collapse and death.
Most cases of thyrotoxicosis aren’t preventable.
If you’re taking thyroid medication (levothyroxine), you can prevent thyrotoxicosis by never taking more than your healthcare provider prescribes. Taking too much thyroid medication can lead to thyrotoxicosis. It’s also important to store your medication safely away from children and pets.
If you’re experiencing symptoms of thyrotoxicosis, it’s important to see your healthcare provider so they can figure out the cause and recommend proper treatment.
Advertisement
If you have chronic thyrotoxicosis (usually a form of hyperthyroidism), you should see your provider regularly to make sure your treatment is working well.
If you’ve received a thyrotoxicosis diagnosis, it may be helpful to ask your provider the following questions:
Although it may sound scary, thyrotoxicosis is a manageable and treatable condition. If you’re experiencing symptoms of thyrotoxicosis — like your bodily functions are going too fast — see your healthcare provider. They can have you undergo some simple tests and recommend treatment to get your body back into balance.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s experienced healthcare providers treat all kinds of thyroid disorders, including issues that cause hypothyroidism and hyperthyroidism.
