A pulmonary embolism (PE) is a blood clot in your lung that creates a blockage. This causes issues with blood flow and oxygen levels in your lungs. A PE is a medical emergency. You need a prompt diagnosis and treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
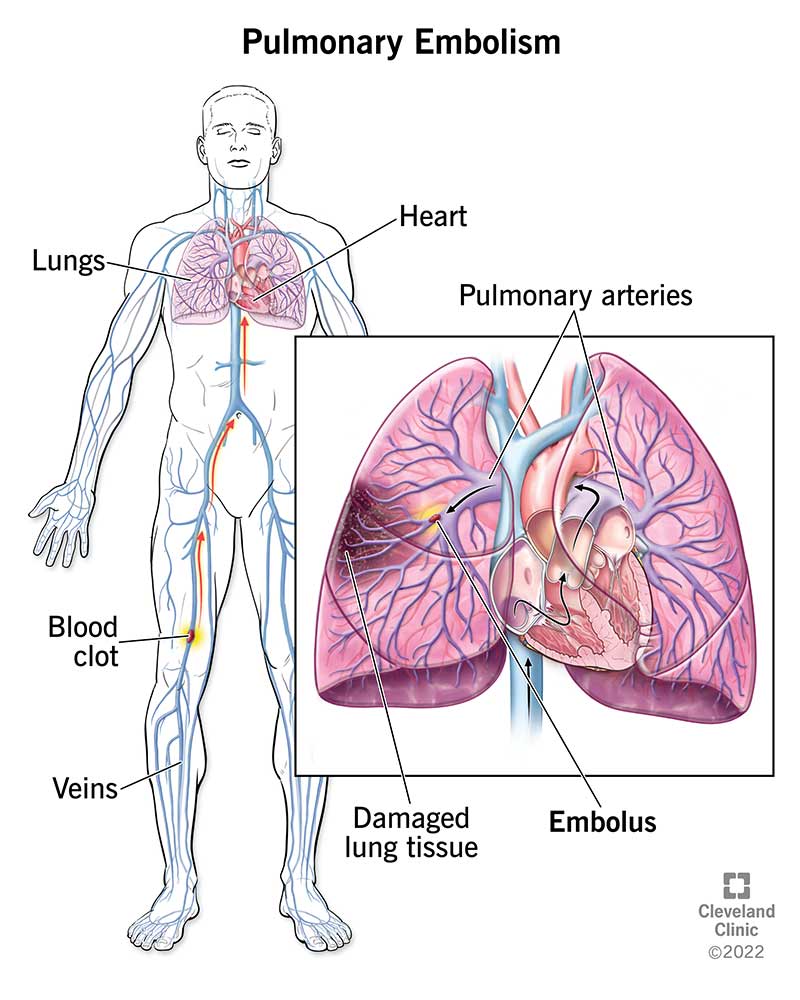
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17400-pulmonary-embolism-illustration.ashx)
A pulmonary embolism (PE) is a blood clot in one of the blood vessels in your lung. This happens when a clot in another part of your body (often your leg or arm) moves through your veins to your lung. A PE restricts blood flow to your lungs, lowers oxygen levels in your lungs and increases blood pressure in your pulmonary arteries.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This condition is a medical emergency. Without quick treatment, a pulmonary embolism can cause heart or lung damage and even death. About 33% of people with a pulmonary embolism die before they get a diagnosis and treatment.
A pulmonary embolism can:
With timely diagnosis and treatment, a PE is seldom fatal.
Pulmonary embolism is one of the most common heart and blood vessel diseases in the world. It ranks third behind heart attack and stroke. In the United States, about 900,000 people a year get a PE.
The first signs of pulmonary embolism are usually shortness of breath and chest pains that get worse if you exert yourself or take a deep breath.
If you have these symptoms, get medical attention right away. Pulmonary embolism is serious but very treatable. Quick treatment greatly reduces the chance of death.
Pulmonary embolism symptoms can vary, depending on the severity of the clot. Although most people with a pulmonary embolism experience symptoms, some don’t.
Pulmonary embolism symptoms may include:
Advertisement
If you have any symptoms of a pulmonary embolism, get medical attention immediately.
Some people have mild symptoms that appear over a number of days or even weeks. Over time, the symptoms get worse and get your attention. But some people get symptoms just minutes (or even seconds) after a pulmonary embolism happens.
Pulmonary embolism causes include:
People at risk of developing a PE include those who:
If you have any of these risk factors and you’ve had a blood clot, talk with your healthcare provider so they can take steps to reduce your risk of PE.
A pulmonary embolism can lead to:
After looking at your symptoms and risk factors, a provider will use the following tests to make a PE diagnosis:
Other tests your provider may order include:
Healthcare providers usually treat a PE in a hospital, where they can monitor your condition closely.
The length of your pulmonary embolism treatment and hospital stay will vary, depending on the severity of the clot. Some people may not need to stay overnight.
Advertisement
The main treatment for a pulmonary embolism is an anticoagulant (blood thinner).
Depending on the severity of your clot and its effect on your other organs such as your heart, you may also undergo thrombolytic therapy, surgery or interventional procedures to improve blood flow in your pulmonary arteries.
Anticoagulant medications
In most cases, treatment consists of anticoagulant medications (blood thinners). Anticoagulants decrease your blood’s ability to clot. This prevents future blood clots.
As with any medicine, it’s important to understand how and when to take your anticoagulant and follow your provider’s guidelines.
Your diagnosis will determine the type of medication you’ll take, how long you need to take it, and the type of follow-up monitoring you’ll need. Be sure to keep all scheduled follow-up appointments with your provider and the laboratory so they can monitor your response to the medication.
While taking anticoagulants, your follow-up may include frequent blood tests (prothrombin time test) to see how fast your blood clots. This helps your provider know if you’re taking the right dose.
Compression stockings
Compression stockings (support hose) improve blood flow in your legs. People with deep vein thrombosis often use them. You should use them as your provider prescribes. The stockings are usually knee-high length and compress your legs to prevent your blood from pooling.
Advertisement
Talk with your provider about how to use your compression stockings, for how long and how to care for them. It’s important to wash compression stockings according to directions to prevent damaging them.
Procedures
If a PE is life-threatening, or if other treatments aren’t working, your provider may recommend using surgery or a catheter to remove the blood clot from your pulmonary artery. Thrombolytic therapy is another option. Your healthcare provider may also recommend an interventional procedure in which a provider places a filter inside your body’s largest vein. A vena cava filter traps clots before they enter your lungs.
Thrombolytic therapy
Thrombolytic medications (“clot busters”), including tissue plasminogen activator (TPA), dissolve the clot. You’ll always receive thrombolytics in the emergency department or intensive care unit (ICU) of a hospital where a provider can monitor you. You may receive this type of medication if you have a special situation, like low blood pressure or an unstable condition because of the pulmonary embolism.
Bleeding is a possible side effect of medications for pulmonary embolism treatment. A provider will give you the dose of anticoagulants or thrombolytics that fits your situation. Keeping you in the hospital allows them to monitor your condition.
Advertisement
You should feel better within a week of treatment. But a pulmonary embolism can take months or years to go away completely.
Your heart has to work harder to push against restricted blood flow and higher blood pressure from a PE. Because of this, some people also have issues with getting one of their heart chambers back to normal months later. This makes them less able to handle as much physical activity as they did before they had a pulmonary embolism.
Without treatment, a pulmonary embolism is a very serious condition that can lead to permanent illness or death. Some people die suddenly or a few hours after a pulmonary embolism happens. This can happen before a provider makes a diagnosis.
Your risk of dying from a PE is higher if you have a heart or lung condition. Still, with better imaging methods than providers had in the past, a pulmonary embolism is fatal for only about 1% to 3% of people who have one.
With treatment, your prognosis (outlook) depends on the size of the blood clot and blockages, as well as your overall health and how well your heart can pump blood.
It can take months or years for a pulmonary embolism to go away completely. Chronic thromboembolic pulmonary hypertension (CTEPH) is a chronic manifestation of PEs that keep coming back.
Yes, you may be able to prevent it. Ways to prevent a pulmonary embolism include:
You’ll need to take a blood thinner for three to six months or longer. Don’t stop taking it unless your provider instructs you to. If you’re taking a blood thinner, don’t do things that put you at risk of an injury that could make you bleed.
Be sure you discuss and understand your follow-up care with your healthcare provider. Follow their recommendations to reduce the risk of another PE. They may suggest you stop using tobacco products, get more physical activity and consider changing your eating habits.
Keep all appointments with your provider and the laboratory so they can monitor your response to prescribed treatments.
If you’re feeling anxious or fearful after your PE, ask your provider about talking to a counselor who can help.
See your healthcare provider for follow-up appointments. While taking a blood thinner, contact your provider if you have black poop, a bad headache or a bruise that’s getting bigger. These signs could mean that you’re bleeding internally.
Get immediate treatment if you have pulmonary embolism symptoms. (See symptoms section above.)
Questions you may want to ask your provider include:
After you survive a pulmonary embolism, you may be surprised to find that your life may not just go back to the way it was before. It’s OK to admit that you’ve been through something difficult. People might not understand why you’re afraid it’ll happen again. It can help to talk through your fears with a support group or a counselor. To fight your fears, keep following your provider’s recommendations. That includes taking medicines they prescribe for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A blood clot in your lungs is serious. But Cleveland Clinic has the expert pulmonary embolism treatment you need.
