Varicose veins are swollen veins that appear just under the skin in your legs, feet or ankles. When your vein walls are weak and your valves aren’t working right, blood backs up in your vein. This causes blue and purple bulges. Treatments can work, but varicose veins can return. For most people, varicose veins aren’t a major problem.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
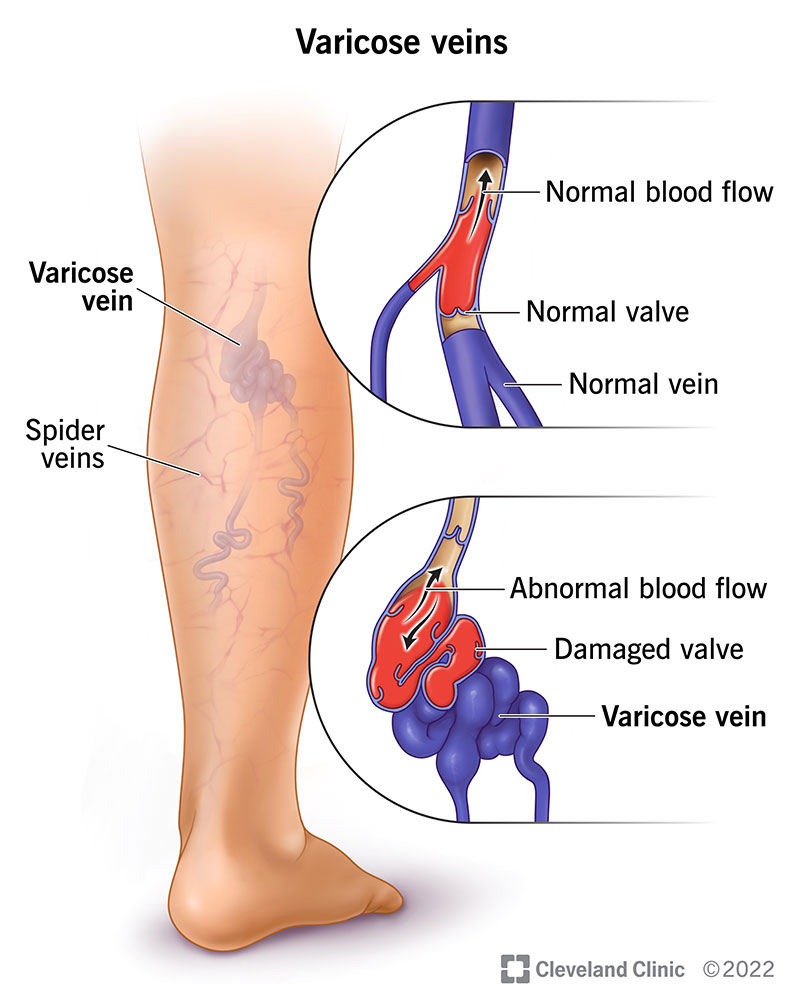
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4722-varicose-veins-illustration)
Varicose veins are swollen, engorged blood vessels that bulge just under your skin’s surface. These blue or purple bulges usually appear in your legs, feet and ankles. They can be painful or itchy. Spider veins, which may surround varicose veins, are smaller red or purple lines that appear close to your skin’s surface.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You may not like the way varicose veins look or feel, but they aren’t dangerous for most people. In some cases, severe varicose veins can lead to serious health problems, like blood clots. You can relieve most varicose vein symptoms at home. If you have a more serious case, you may need treatment with injections, laser therapy or surgery from your healthcare provider.
Varicose veins are very common.
The most recognizable sign of varicose veins is a gnarled, blue or purple vein just under your skin’s surface. Varicose vein symptoms include:
Advertisement
Most often, varicose veins develop on the lower half of your body, usually on your calves, ankles and feet. They can also develop in the pelvic area (pelvic congestion syndrome), especially in people who’ve had children. Hemorrhoids, which form in your rectum, are also varicose veins.
Varicose veins occur when the walls of your veins weaken. As blood pressure in your vein increases, the weakened walls allow your vein to get bigger. As your vein stretches, the valves that keep blood moving in one direction in your vein can’t work as they should. The sluggish blood backs up or pools in your vein, causing your vein to swell, bulge and twist.
Vein walls and valves can become weak for several reasons, including:
Anyone can develop varicose veins. Certain factors increase your chances of developing a varicose vein, including:
Most people don’t have complications from varicose veins. But in some people, an untreated varicose vein can cause ulcers (open sores), bleeding, inflammation or skin discoloration. Severe varicose veins may be a sign of chronic venous insufficiency (CVI). This condition affects your veins’ ability to pump blood to your heart.
If you have varicose veins, you may be more likely to develop blood clots. It’s important to tell your healthcare provider about varicose veins so they can evaluate and monitor you for clotting disorders. These include:
Varicose veins are close to the surface of your skin and easy to see. Healthcare providers can diagnose the condition during a physical examination. They’ll feel your veins and examine them while you’re sitting and standing. They may also ask you questions about your medical history and your symptoms.
Advertisement
Providers usually don’t need additional diagnostic tests to diagnose varicose veins. To see detailed images of your veins and check for complications, your provider may recommend an ultrasound. This safe, painless test uses sound waves to produce pictures of tissues inside your body. Ultrasounds can show blood clots and how your valves are working.
Although there isn’t a cure for varicose veins, treatments can help you look and feel better. And you’ll most likely go home the same day as your procedure. Varicose vein treatments include:
Advertisement
Potential side effects of these treatments include:
Although treatments are effective, varicose veins can return. They’re more likely to come back in people who become pregnant after treatment. You have a higher chance of varicose veins reappearing if you have obesity (a BMI, or body mass index, over 30) or a sedentary lifestyle.
Usually, varicose veins aren’t dangerous and don’t cause long-term health problems. Most people with the condition are concerned with the way varicose veins look. They may experience discomfort but don’t develop complications.
Most of the time, varicose veins that happen while you’re pregnant go away on their own within two or three weeks after you have your baby. For other people, varicose veins may keep coming back after treatment.
You may not be able to prevent varicose veins. But you can reduce your chances of developing them by living an active, healthy lifestyle. Healthcare providers recommend many of the same measures to prevent and treat varicose veins:
Advertisement
You can take care of yourself in several ways, like:
Although varicose veins aren’t usually dangerous, you should visit your healthcare provider for an exam. If you’re concerned about how varicose veins look, or if they’re uncomfortable, treatments can help. You should see your provider as soon as possible if the skin or veins are:
Millions of people live with varicose veins. For most, varicose veins don’t cause serious health problems. Lifestyle changes and at-home remedies can relieve symptoms and prevent them from getting worse. Talk to your healthcare provider about safe, minimally invasive treatments that can reduce pain and improve the appearance of varicose veins.
Call 911 or your local emergency number if you have a varicose vein that’s bleeding heavily.
Questions to ask your provider may include:
Varicose veins may keep you from wearing shorts and even cause you discomfort. The good news is that many people don’t have complications from the condition. If varicose veins bother you, you can try home treatments that may help. Or you can ask your healthcare provider about different available treatments. Just keep in mind that varicose veins can happen again, even after treatment. Talk to your provider about which treatment is best for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Vascular disease may affect your life in big and small ways. Cleveland Clinic’s specialists treat the many types of vascular disease so you can focus on living.
