Mammograms are an essential breast cancer screening and diagnostic tool. Using low-dose X-rays, they can show abnormal areas in your breast tissue. It can help detect changes that could lead to breast cancer before you have symptoms. Most females should begin getting mammograms at age 40, although your age and frequency depends on your risk.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_zfs3jhcm/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Early detection is key when it comes to diagnosing and treating breast cancer.
A mammogram is a low-dose X-ray of your breast tissue. Healthcare providers use mammograms, or mammography, to look for early signs of breast cancer before symptoms develop. This is called a screening mammogram. Providers also use mammography to look for any abnormalities if you develop a new symptom, such as a lump, pain, nipple discharge or breast skin changes. This is called a diagnostic mammogram.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Aside from skin cancer, breast cancer is the most common cancer that affects females and represents 15% of all new cancer diagnoses in the United States. An early diagnosis plays a big role in your breast cancer survival rate. Routine mammograms are key to catching breast cancer early. When breast cancer is detected early, the five-year survival rate is 99%. Mammograms are the gold standard in detecting breast tissue changes before they turn into cancer.
There are two main types of mammograms:
2D mammography involves taking pictures of each breast at two different angles — typically from top to bottom and side to side.
3D mammography is a newer type of mammogram in which each breast is compressed once and a machine takes several X-rays as it moves in an arc over your breast. A computer then puts the images together in “slices,” which allows healthcare providers to see your breast tissues in 3D.
Mammograms can help detect cancer, but they can’t diagnose cancer.
While mammograms can show abnormal breast tissue, they can’t prove that an abnormal area in your breast is cancer. Rather, mammograms are an essential tool for helping healthcare providers decide whether you need additional testing, such as a breast biopsy. A breast biopsy can determine if tissue is cancerous or noncancerous.
Advertisement
The U.S. Preventive Services Task Force recommends that all females receive mammograms every two years beginning at age 40 until they reach age 75. Other medical groups have different recommendations. Talk with your healthcare provider about what recommendation is right for you.
If you have a higher risk of developing breast cancer, you may need to have screening mammograms before age 40, or more frequently. Your provider may also recommend supplemental screening with other tests, such as a whole breast ultrasound or breast MRI (magnetic resonance imaging).
Your healthcare provider can perform a breast cancer risk assessment to determine if you’re at a higher risk. If you have any of the following risk factors, talk to your provider about when you should start getting annual screening mammograms:
Occasionally, males may also have a high-risk level because of their family history and may also have screening mammography. In general, though, about 1 out of 100 breast cancers occur in males.
How often you need to get a mammogram depends on your risk. If you have an average risk of developing breast cancer, you should get a mammogram every one to two years beginning at age 40. If your risk is higher, you may begin mammograms sooner or need them more often. Talk to your healthcare provider about your mammography schedule, which is based on your medical history and other factors.
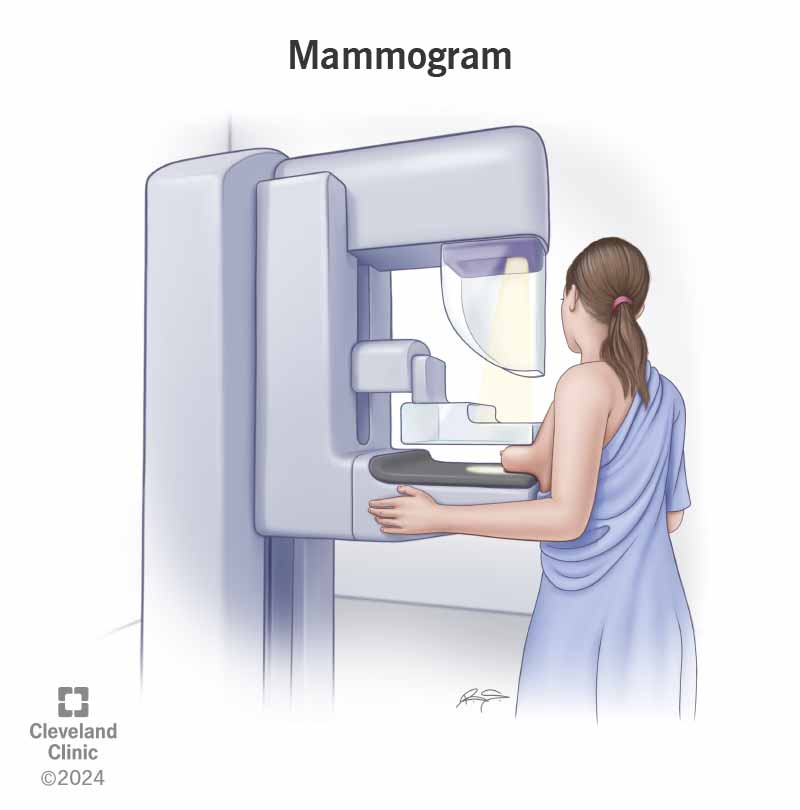
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4877-mammogram-illustration)
A mammogram uses an X-ray machine that’s made specifically for breast tissue. The machine takes X-rays at lower radiation doses than the X-rays that look at your bones.
During a mammogram, you place your breast on a support plate attached to the X-ray machine. A technologist then squeezes your breast with a parallel plate called a paddle. The machine produces X-rays that pass through your breast to a detector located on the opposite side. The detector transmits electronic signals to a computer to form a digital image. These images are called mammograms.
Breast compression is necessary for a mammogram to hold your breast still and minimize movement, which can cause the X-rays to look blurry. Compression also evens out the shape of your breast so that the X-rays can travel through a shorter path to reach the detector. This allows for a lower radiation dose and improves the quality of the image.
Advertisement
A healthcare provider called a radiology technologist or a mammographer performs a mammogram. They have special training in performing a mammogram safely and properly. A board-certified physician radiologist who’s specially qualified to interpret mammograms then views and analyzes the mammogram images. They send the results to your healthcare provider, who will then share them with you.
There are a few things to do or keep in mind when scheduling your mammogram, including:
On the day of your mammogram, follow these guidelines:
Advertisement
A mammogram involves the following steps:
Advertisement
Most people will be able to resume their normal activities immediately after their mammograms.
Having a mammogram feels uncomfortable for some people due to the pressure on your breast tissue from the compression. For some, it’s painful. The good news is that a mammogram is a brief procedure, and the discomfort doesn’t last long. If you feel intense pain, tell the technologist immediately.
The level of discomfort you may feel depends on a few factors, including:
Screening mammograms usually take about 15 to 20 minutes. Diagnostic mammograms may take longer due to your provider needing to take extra images.
Mammograms expose your breasts to small amounts of radiation, but the benefits of mammography outweigh any possible harm from the radiation exposure.
If there’s any chance you might be pregnant, let your healthcare provider and technologist know. Although mammograms are safe during pregnancy, healthcare providers may recommend postponing screening mammograms if you don’t have an increased risk of developing breast cancer and are pregnant.
You’ll likely get your mammogram results within a few days, although this can vary. Often, radiologists compare your most recent mammogram to your last mammogram. Once they review your mammogram, they send the results to you and your healthcare provider.
Contact your provider or the facility where you got your mammogram if you don’t receive your results within a month.
You’ll receive a result letter that gives basic information about the result and should be easy to understand. The letter may inform you of normal results or the need to return for additional imaging. Your mammogram report will also include information about your breast density, which is how much fibrous and glandular tissue you have in your breasts as compared to fatty tissue. This information is now mandated by law to be provided in your report. If you have any questions about your results, don’t be afraid to ask your healthcare provider.
Radiologists and healthcare providers use a standard system in medical reporting to describe screening and diagnostic mammogram findings called the Breast Imaging Reporting and Data System (BI-RADS). This system sorts the results into categories numbered 0 through 6. The system gives you your category, the finding and the explanation (including your risk for cancer).

Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/bi-rads-chart)
BI-RADS is a system to categorize and define breast imaging results.
If you have a normal mammogram, it means that the radiologist didn’t find any issues or abnormal areas in your breasts in the images. If you have a normal mammogram, it’s important to continue to get mammograms at the interval your healthcare provider recommends. Screening mammograms are most helpful when a radiologist can compare them to ones you’ve had in the past to look for changes in your breasts.
If a mammogram shows one or more suspicious regions, the radiologist will likely recommend additional specialized mammogram images — or other imaging tests such as a breast ultrasound or a breast biopsy.
Your healthcare provider will go over the next steps with you if you receive an abnormal mammogram report.
Mammography is 85% to 90% accurate. Mammograms have improved the ability to detect breast abnormalities before you can see them or feel them. But it’s still possible that an abnormality doesn’t show up on a mammogram.
It’s important to contact your healthcare provider right away if you feel something suspicious when self-examining your breasts or if you have any new breast symptoms.
Having silicone or saline breast implants and resulting scar tissue makes it more difficult for radiologists to see all of your breast tissue and possible issues on regular mammograms.
To help the radiologist see as much breast tissue as possible, people with implants usually have two extra pictures done on each breast, in addition to the four standard pictures taken during a screening mammogram. These extra images are called implant displacement (ID) views.
For ID views, the technologist gently pushes your breast implant back against your chest wall, pulls your breast forward over it and then compresses your breast. This allows for better imaging of the front part of each breast.
It’s important to let the mammogram facility know if you have breast implants when scheduling your mammogram and to let your technologist know on the day of your mammogram.
Mammograms are an essential breast cancer screening tool. They can also help monitor benign breast conditions over time. While the procedure can be uncomfortable and waiting for results can be anxiety-inducing, it’s important to get your mammogram at the recommended age and time intervals based on your risk of developing breast cancer. If you have any questions about your risk of getting breast cancer or the mammogram process, talk to your healthcare provider. They’re there to help you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A mammogram is a way to keep track of changes in your breasts. Cleveland Clinic’s experts can help you get a mammogram and connect you to the care you need.
