Breast cancer screening detects cancer and saves lives. Mammograms have been the best tool for a long time. When combined with digital breast tomosynthesis, or DBT (3D mammograms), mammograms are far more likely to detect cancer, especially in dense breast tissue.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
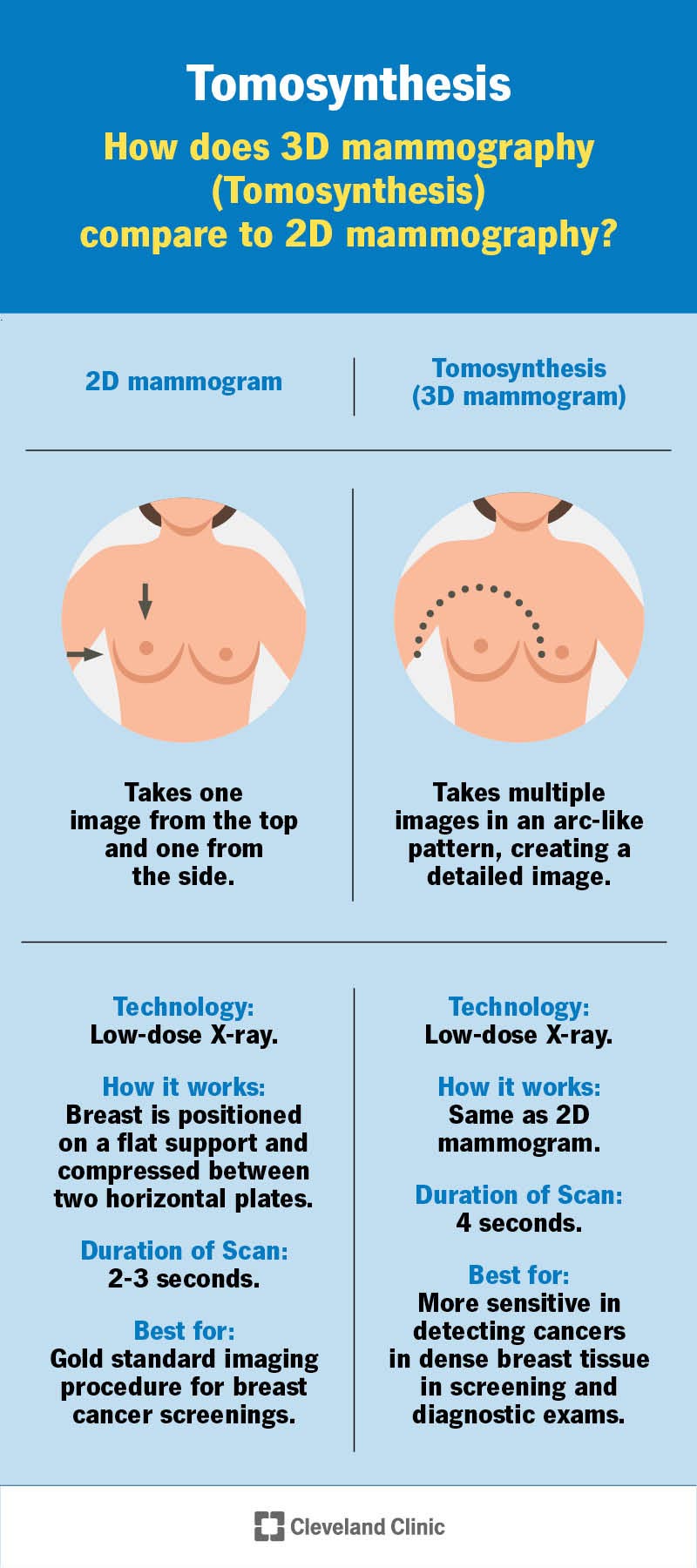
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/15939-tomosynthesis)
Digital breast tomosynthesis (pronounced “toh-moh-SIN-thah-sis”) is a technologically advanced mammogram that’s excellent at detecting breast cancer, especially in dense breast tissue. Breast tomosynthesis is also known as 3D mammography because it uses a series of two-dimensional images to build a three-dimensional image of your breast. Standard mammography, still considered the most reliable procedure for breast cancer screenings, takes 2D images of breasts.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The U.S. Food and Drug Administration (FDA) approved digital breast tomosynthesis (DBT) in 2011. Given how effectively DBT detects cancer, it may eventually become the new gold standard in breast imaging.
Anyone who needs a mammogram can potentially benefit from DBT, but it’s especially beneficial if you have dense (as opposed to fatty) breast tissue. About half of women have dense breasts. The denser your breast tissue, the harder it is to spot cancer on a standard 2D mammogram.
Like standard mammograms, DBT uses low-dose X-rays to take images of the inside of your breast. Dense (thick or compacted) tissue — including bone, solid tumors and dense breast tissue — absorbs more radiation from the X-ray, making it appear white on a mammogram. Distinguishing between cancer and dense breast tissue can be tricky, as they both appear white on imaging.
Digital breast tomosynthesis takes multiple pictures of your breast from more angles than a standard mammogram, creating a more detailed image. DBT reveals cancers that may have otherwise been “hidden” in dense breast tissue. It correctly identifies normal tissue that may appear “suspicious” or potentially cancerous on a standard mammogram. In this way, DBT decreases the frequency of a false-positive result (learning that you may have cancer when you really don’t).
Advertisement
Digital breast tomosynthesis is a:
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_zfs3jhcm/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Early detection is key when it comes to diagnosing and treating breast cancer.
A radiologic technologist or mammographer will position you for the procedure and operate the mammography machine. A radiologist will analyze the images and communicate test results with your referring provider.
Digital breast tomosynthesis (DBT) is similar to a standard mammogram. The major difference is that it takes more pictures of your breast from more angles to capture more detail.
During a standard mammogram, your breast is positioned on a flat support and compressed (squeezed) between two horizontal plates. The machine takes 2D images of your breast from two angles, top to bottom and side to side.
During DBT, your breast is positioned and compressed the same way it is for a 2D mammogram. However, during breast tomosynthesis, the arm of the mammogram machine (X-ray tube) moves in an arc over your breast, taking many 2D images from multiple angles as it moves.
The 2D images get digitized and fed into a computer that combines them into a 3D image. The 3D image shows more details, making it easier to tell the difference between healthy and potentially cancerous tissue.
Ensure your healthcare provider is fully informed about your medical history — especially your breast health. To prepare:
Advertisement
Plan for the procedure to take about 30 minutes. You’ll go home that same day. To prepare:
Having DBT is like having a standard mammogram. The biggest difference is that with DBT, the arm of the machine (X-ray tube) moves in a slow arc around your breast as it takes the X-rays.
Advertisement
The FDA has approved DBT to be used only in combination with mammography. The total radiation dose is just under three times that of a mammogram. While three times may sound like a lot, it’s still a low dose of radiation that’s considered a safe amount of radiation exposure.
Newer tomosynthesis techniques can create 2D images from the data used to make the 3D image. This lowers the radiation exposure so it’s only slightly higher than a standard mammogram.
Mammography, including tomosynthesis, uses the lowest, safest radiation dose possible that still produces a high-quality image for breast cancer detection.
A radiologist will examine the images to check for signs of breast cancer. They may compare the 3D image to your previous mammogram results or the 2D images if they notice a suspicious area. They’ll prepare a report for your provider, who’ll share the results with you.
Depending on the results, you may receive confirmation that you don’t have cancer. You may learn that you need additional tests to check suspicious tissue more closely. You may need an additional mammogram, an ultrasound, MRI or a biopsy. A biopsy is the only way to confirm a cancer diagnosis.
You’ll likely get results within a few days, but it may take longer. Before leaving the testing facility, ask about how you’ll receive results and when you should expect them.
Advertisement
Tomosynthesis produces a more detailed image of your breast than a standard mammogram. It’s better at detecting cancer and reducing false-positive results in dense breast tissue. Still, research is ongoing about whether 3D mammograms are better than 2D mammograms when it comes to breast cancer screening in general.
Follow your healthcare provider’s recommendations on which breast imaging procedures you need based on your medical history and breast tissue.
Yes. Tomosynthesis, breast tomosynthesis, digital breast tomosynthesis and 3D mammograms are all the same imaging procedures.
Yes. It provides a more detailed image of your breast, making it easier for a radiologist to tell the difference between dense breast tissue and cancer.
Digital breast tomosynthesis (DBT) may be the best option for detecting breast cancer if you have dense breast tissue. If you’re due for a mammogram, ask your healthcare provider whether tomosynthesis will be part of the procedure. Depending on your health, a standard mammogram may be enough for breast cancer detection. In some cases, tomosynthesis may be more likely to detect cancer or eliminate the stress of a false-positive result. Don’t hesitate to ask for details about the procedure, including why it is (or isn’t) right for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
A breast cancer diagnosis can turn your world upside down. At Cleveland Clinic, we offer expertise, compassion and personalized treatment plans.
