The male reproductive system mostly exists outside of your body. The external organs include your penis, scrotum and testicles. Internal organs include your vas deferens, prostate and urethra. The male reproductive system is responsible for sexual function and urination.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
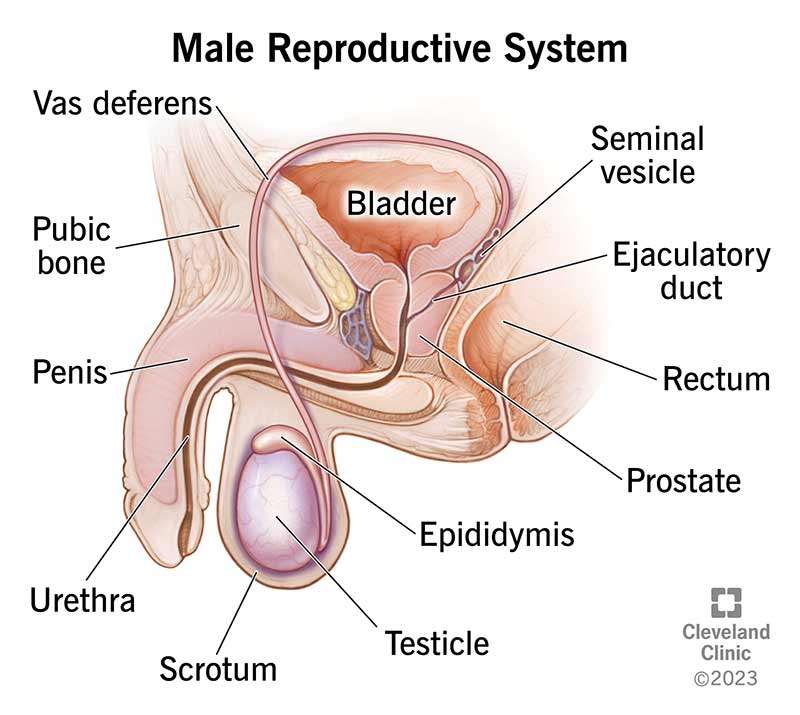
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/9117-male-reproductive-system)
The male reproductive system consists of a group of organs that make up the reproductive system and urinary system.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The male reproductive system contains internal and external parts. Internal parts are inside your body, and external parts are outside your body. Together, these organs help you pee, have sexual intercourse and make biological children.
The organs that make up the male reproductive system perform the following:
The entire male reproductive system depends on hormones. Hormones are chemicals that stimulate or regulate activity in your cells or organs. The primary hormones that help the male reproductive system function include:
Most of the male reproductive system is on the outside of your abdominal cavity or pelvis. The external body parts include your penis, scrotum and testicles. Other names for these parts are genitals or genitalia.
Advertisement
The penis is the male organ for sexual intercourse. It contains many sensitive nerve endings, and it has three parts:
In most people, the opening of the urethra is at the tip of the glans. The urethra transports pee and semen out of your body. Semen contains sperm. You expel (ejaculate) semen through the end of your penis when you reach sexual climax (orgasm).
When your penis is erect, your corpora cavernosa press against the part of your urethra where pee flows. This blocks your pee flow so that only semen ejaculates when you orgasm.
Studies suggest that the average penis is about 3.5 inches (8.9 cm) when flaccid (soft) and a little more than 5 inches (13 cm) when erect.
Your scrotum is the loose, pouch-like sac of skin that hangs behind your penis. It holds your testicles (testes) as well as nerves and blood vessels.
Your scrotum protects your testicles and provides a sort of “climate-control system.” For normal sperm development, your testes must be at a temperature that’s slightly cooler than body temperature (between 97 and 99 degrees Fahrenheit or 36 and 37 degrees Celsius). Special muscles in the wall of your scrotum let it contract (tighten) and relax. Your scrotum contracts to move your testicles closer to your body for warmth and protection. It relaxes away from your body to cool them.
Your testicles (testes) are oval-shaped organs that lie in your scrotum. They’re about the size of two large olives. The spermatic cord holds your testicles in place and supplies them with blood. Most people have two testicles, on the left and right side of their scrotum. Your testicles make testosterone and produce sperm. Within your testicles are coiled masses of tubes. These are the seminiferous tubules. The seminiferous tubules produce sperm cells through spermatogenesis.
Advertisement
Your epididymis is a long, coiled tube that rests on the back of each testicle. It carries and stores the sperm cells that your testicles create. Your epididymis also brings the sperm to maturity — the sperm that emerge from your testicles are immature and incapable of fertilization. During sexual arousal, muscle contractions force the sperm into your vas deferens.
There are several internal (accessory) organs in the male reproductive system. They include:
Your vas deferens is a long, muscular tube that travels from the epididymis into your pelvic cavity, just behind your urinary bladder. Your vas deferens transports mature sperm to the urethra in preparation for ejaculation.
Each testicle has a vas deferens that joins with seminal vesicle ducts to form ejaculatory ducts. The ejaculatory ducts move through your prostate, where they collect fluid to add to semen. They empty into your urethra.
The urethra is the tube that carries pee from your bladder outside of your body. If you have a penis, it also ejaculates semen when you reach orgasm.
Your seminal vesicles are sac-like pouches that attach to your vas deferens near the base of your bladder. Seminal vesicles make up to 80% of your ejaculatory fluid, including fructose. Fructose is an energy source for sperm and helps them move (motility).
Advertisement
Your prostate is a walnut-sized gland that rests below your bladder, in front of your rectum. Your prostate adds additional fluid to ejaculate, which helps nourish sperm. Your urethra runs through the center of your prostate gland.
Your bulbourethral glands are pea-sized structures on the sides of your urethra, just below your prostate. They create a clear, slippery fluid that empties directly into your urethra. This fluid lubricates your urethra and neutralizes any acids that may remain from your pee.
Common conditions that affect the male reproductive system include:
Common signs of conditions that affect the male reproductive system include:
A healthcare provider may order the following tests to check the health of the male reproductive system:
Advertisement
No, a man can’t go through menopause.
Menopause is when the ovaries stop making reproductive hormones. One of the biggest changes after menopause is a stop to menstruation. This means a female can't have biological children any more. In males, the testicles don’t lose the ability to make hormones. Males may be able to make sperm well into their 80s or even longer.
However, subtle changes in how your testicles function can happen when you’re around 45. The changes can happen more dramatically after 70. Some people refer to this as “male menopause.” For many males, hormone production remains normal into their 60s and longer. Declining hormone function at an earlier age may be a side effect of another condition, like diabetes.
It’s not clear whether decreasing testicular function contributes to other symptoms, like erectile dysfunction, fatigue, weakness or depression.
If your testosterone levels are low, hormone replacement therapy may help relieve some symptoms, including low sex drive, depression and fatigue. However, replacing male hormones can make prostate cancer worse. It can also make atherosclerosis worse.
Talk to a healthcare provider about all the pros and cons of hormone replacement therapy. Before starting, you should get a complete physical examination and laboratory tests.
As you age, your testicles (balls) may shrink, and your scrotum may hang lower.
The male reproductive system includes many different organs. Many people think of their external organs, which include their penis, scrotum and testicles. However, the male reproductive system also includes many internal parts, including the urethra and prostate. Together, the parts that make up the male reproductive system involve sexual activity, reproduction and peeing. Your external reproductive organs might look different than someone else’s, and it’s natural for them to change slightly over time. However, if you have any symptoms or concerns about your genitals, talk to a healthcare provider.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a condition that’s affecting your urinary system, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
