Typically, you have a vas deferens (also called a sperm duct or a ductus deferens) in each testicle. The job of these ducts is to move sperm away from its storage place in the testicle. The ducts can be affected by scar tissue or infections.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
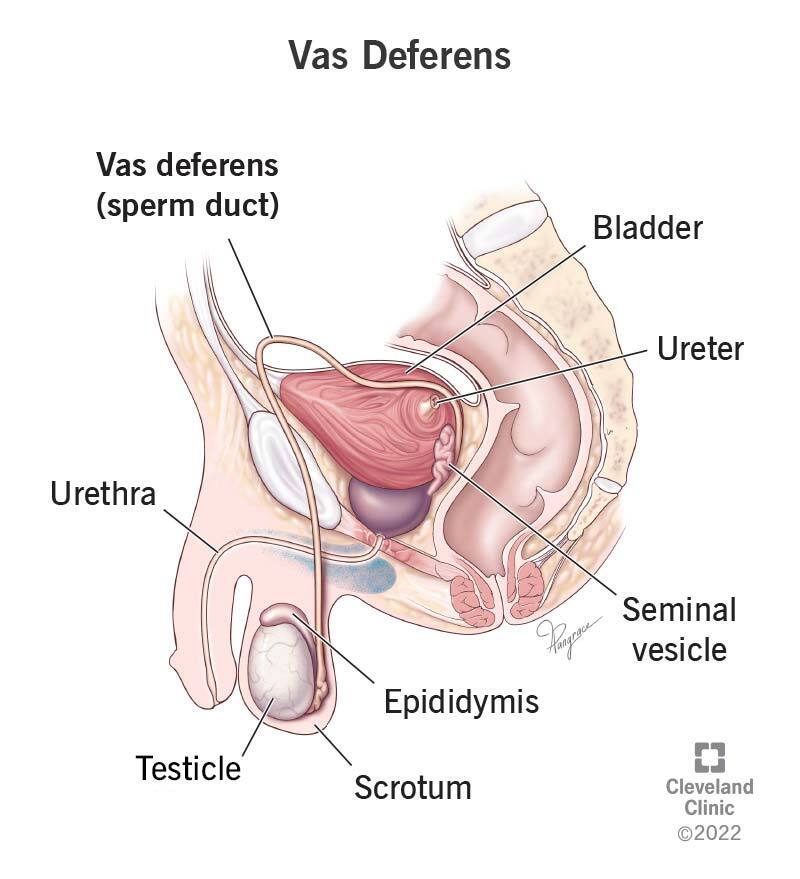
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22763-vas-deferens)
Your two vasa deferentia (plural) are part of the male reproductive system. The vas deferens (singular) is also called a ductus deferens or a sperm duct. This long muscular tube runs from the epididymis into the pelvic cavity behind your bladder and connects to your urethra through a structure called the ejaculatory duct. Your vas deferens is surrounded by your spermatic cord and transports mature sperm to the urethra before you ejaculate.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your testes are the place where sperm cells are created. From there, the sperm moves into the epididymis, which is a structure located on top of the testicle. The epididymis stores sperm cells and has the job of bringing them to maturity so they’re able to fertilize eggs.
When you’re sexually aroused, muscle contractions move the sperm from the epididymis to the vas deferens and from there into the urethra so you’re able to ejaculate semen outside of your body. During the process, your body adds secretions to the sperm cells to make semen.
The vas deferens begins in the scrotum, which is the sac containing your testicles. The vas deferens then travels from the testicle into your body. It continues until it joins with the duct of the seminal vesicle to create the ejaculatory duct.
The vas deferens, or ductus deferens, can be 30 centimeters (almost 12 inches) to 45 centimeters (almost 18 inches) long. Some parts of it are coiled, but other parts are straight. The tube is described as being fibromuscular, meaning that it’s made of fibrous tissue and muscle tissue.
Conditions that may affect your vas deferens include:
Advertisement
While not really a condition, a vasectomy will affect each vas deferens. During the procedure, your surgeon will cut or burn the sperm duct in each testicle. This will stop sperm from leaving your body and is designed to be a permanent form of birth control.
Some signs and symptoms that you may have a condition that’s affecting your vas deferens include:
After taking your medical history and asking questions about your overall health and possible symptoms, your healthcare provider will do a physical exam. They’ll look at your penis and scrotum and will palpate (touch) them gently.
Your healthcare provider will use each hand to feel each of your testicles at the same time. Your provider knows what a healthy scrotum and spermatic cord feel like, so they can tell if there’s something not quite right.
Your provider may shine a bright light through your scrotum to be able to see if there is a solid mass or a fluid-filled cyst. This is called transillumination.
Your provider may order other tests, including:
Treating your vas deferens depends on what’s causing the illness. Treatments may include:
The tips for keeping yourself healthy will help to keep your reproductive system, including your vas deferens, healthy.
No, but the fallopian tubes serve a similar purpose in the reproductive system typically described as female. The tubes move the eggs from the ovaries to the uterus, where it’s possible that the eggs can be fertilized.
You may never think about your vas deferens unless you have reason to think about it. One reason you may think about your sperm duct is if you’ve been trying to start a family, and you’re unable to do so. Another reason is if you have pain or swelling in the area. It’s important to have a good relationship with your healthcare provider so you can answer their questions honestly. This way, you’ll be able to work together to find a solution.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
