Hypertrophic cardiomyopathy (HCM) causes your heart muscle to enlarge. It’s often genetic. Most people who have it don’t develop complications. But it can be serious for some people. If this is the case for you, there are several treatment options.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
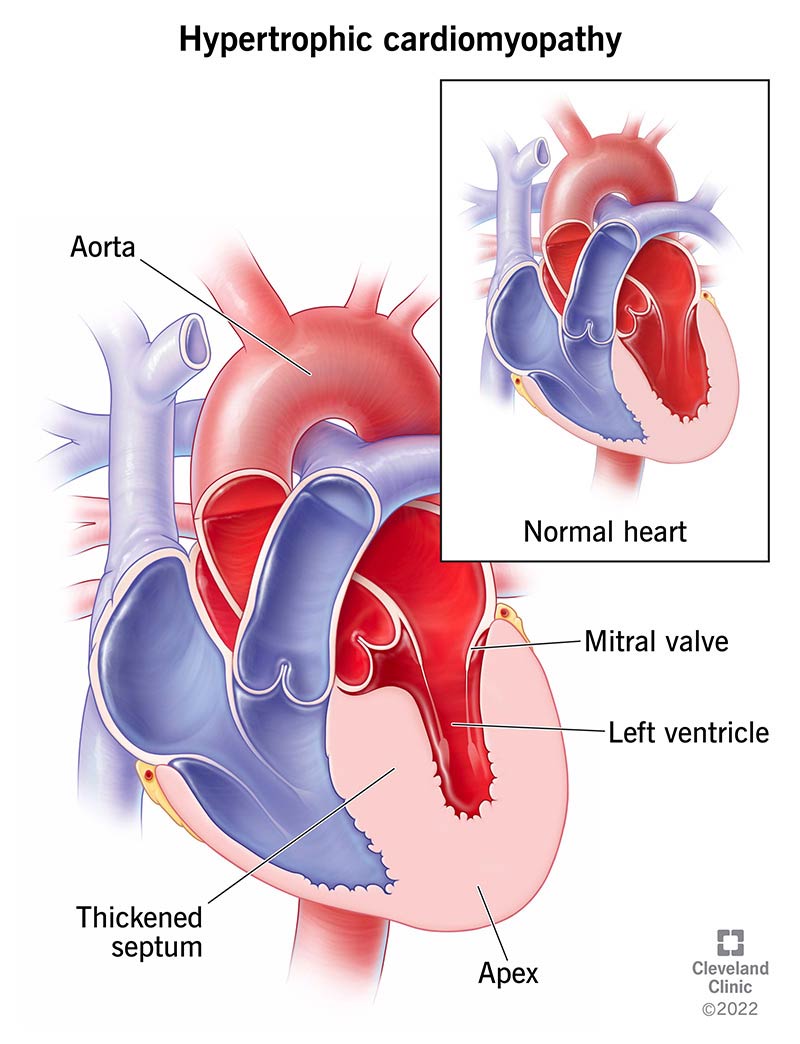
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/17116-hypertrophic-cardiomyopathy)
Hypertrophic cardiomyopathy (HCM) is a complex type of heart disease that thickens your heart muscle. “Hypertrophic” means something is bigger than it should be. “Cardiomyopathy” represents a group of conditions that affect your heart muscle.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The thickening HCM causes can affect any area of your heart’s muscle tissue (myocardium). But HCM most commonly affects the septum — the middle wall that divides your heart into two sides. This makes your heart’s left ventricle have less space to pump blood.
Hypertrophic cardiomyopathy affects about 1 in 500 people in the U.S. But many people don’t know they have it. It’s a lifelong condition that can get worse over time, leading to serious complications. The good news is that early diagnosis and treatment can help prevent complications. Lifestyle changes can also help you stay healthy.
There are two main types of hypertrophic cardiomyopathy:
About 2 in 3 people with HCM have the obstructive type.
Common symptoms of hypertrophic cardiomyopathy include:
Advertisement
You may have several of these symptoms or none at all. If you have them, it’s crucial to see your healthcare provider.
Gene changes cause about 3 in 5 cases of hypertrophic cardiomyopathy. Healthcare providers call this familial HCM. The changes are to genes that are responsible for controlling heart muscle growth. Familial HCM has an autosomal dominant inheritance. This means only one biological parent needs to have an altered gene to pass it on.
Many gene changes can cause hypertrophic cardiomyopathy. Because of this, the severity of HCM can vary widely — even within the same biological family. Some people who have the changed gene may never develop the disease.
Up to 2 in 5 cases of HCM have no known cause. These cases don’t have a gene change that explains the condition. Researchers are currently studying other possible causes of HCM.
HCM can develop at any age. But most people with the condition receive a diagnosis around 40 years of age.
Complications of HCM can include:
Most people with hypertrophic cardiomyopathy don’t experience complications. But because HCM can cause life-threatening health issues, it’s essential to see your cardiologist regularly if you have the condition. It’s also important to get screened for HCM if you have a family history of it.
Healthcare providers can typically diagnose hypertrophic cardiomyopathy based on the following:
Your provider may recommend other tests to help confirm the diagnosis and check for complications. These tests include:
Your provider will also recommend that your first-degree biological family members (parents, siblings and children) get screened for HCM.
Together, you and your cardiologist will decide on a treatment plan based on how HCM is affecting you and your health.
The goal of treatment is to minimize or prevent symptoms and reduce the risk of complications. HCM treatment can include:
Advertisement
If possible, it’s best to receive care through a hospital system that’s experienced in treating hypertrophic cardiomyopathy.
Your cardiologist will assess your risk for complications. If your risk is low and you don’t have symptoms, they may recommend just monitoring your heart and health over time.
Regardless of your risk, your cardiologist will likely recommend a heart-healthy lifestyle. This includes:
Medications that may help improve HCM symptoms include:
A myosin inhibitor (mavacamten) can help improve symptoms and heart function in adults with obstructive HCM. This is the first medication that directly targets the underlying cause of HCM. The U.S. Food and Drug Administration (FDA) approved it in 2022.
Like all medications, these may have certain side effects. Your cardiologist will discuss the risks and benefits with you.
You may also need to take prophylactic (preventive) antibiotics for dental procedures to reduce the risk of bacterial endocarditis.
Advertisement
Procedures that can help treat obstructive hypertrophic cardiomyopathy or prevent complications include:
You’ll need to see your cardiologist regularly so they can check on your heart’s health. HCM is a lifelong condition. They’ll let you know how often you’ll need follow-up appointments based on the severity of HCM and your treatment plan.
If you have HCM, you’ll want to do what you can to protect your heart and overall health. The prognosis (outlook) for HCM varies considerably based on:
Advertisement
Your cardiologist can give you a better idea of what to expect based on your unique situation. Lean on them for guidance and support.
For most people, HCM doesn’t limit their life expectancy. Years ago, mortality (death) rates for people with HCM were 1% to 4%. With treatment, these numbers are now closer to 0.5%.
Most people with HCM have a low risk for complications and an even lower risk for sudden cardiac death. But hypertrophic cardiomyopathy is the most common cause of sudden cardiac death in athletes under age 35.
There’s nothing you can do to prevent hypertrophic cardiomyopathy. But because HCM is often genetic, screening can help catch it early and prevent complications.
It’s important to have screening if you have a biological parent, sibling or child (first-degree relative) with the condition.
The first step is to have an electrocardiogram (EKG) and echocardiogram (echo) to check your heart. If the test results show signs of HCM, you’ll need to see a cardiologist.
It’s possible to have normal test results even if hypertrophic cardiomyopathy runs in your family. In this case, you should have a follow-up echo and EKG every three years until you’re 30 years old, and then every five years after that.
Your cardiologist may tell you to avoid certain medications, like:
Getting a heart disease diagnosis like hypertrophic cardiomyopathy can be overwhelming. Try to take a deep breath. There are ways to manage the condition and protect your health. Your cardiologist will guide you through a thorough management plan. Lean on loved ones for help, too, especially when it comes to lifestyle changes you may have to make.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic offers personalized diagnosis and the latest treatments for hypertrophic cardiomyopathy.
