Considerations for Left Atrial Appendage Closure
Can LAA be performed at the same time as ablation? Can patients with previous valve surgery or ASD safely undergo LAA? When to be concerned with a leak? Drs. Oussama Wazni, Walid Saliba, Mohamed Kanj, and Tyler Taigen discuss considerations for left atrial appendage closure.
Learn more about the Atrial Fibrillation Center and Care Team at Cleveland Clinic.
Subscribe: Apple Podcasts | Buzzsprout | Spotify
Considerations for Left Atrial Appendage Closure
Podcast Transcript
Announcer:
Welcome to Cleveland Clinic Cardiac Consult, brought to you by the Sydell and Arnold Miller Family Heart, Vascular and Thoracic Institute at Cleveland Clinic.
Oussama Wazni, MD, MBA:
Hello, everybody, and welcome once more to a podcast from Cleveland Clinic Electrophysiology. I am Oussama Wazni, the section head of EP here at the Cleveland Clinic.
Oussama Wazni, MD, MBA:
Today, I'm joined with Dr. Walid Saliba, who is the Director of the EP lab and Director of Atrial Fibrillation Center, Dr. Mohamed Kanj, who is the Co-Director of the EP lab and Dr. Tyler Taigen, who is the Director of the Outpatient Department and also Director of our Quality Outcomes Program here at the Cleveland Clinic. Thank you very much for joining us.
Oussama Wazni, MD, MBA:
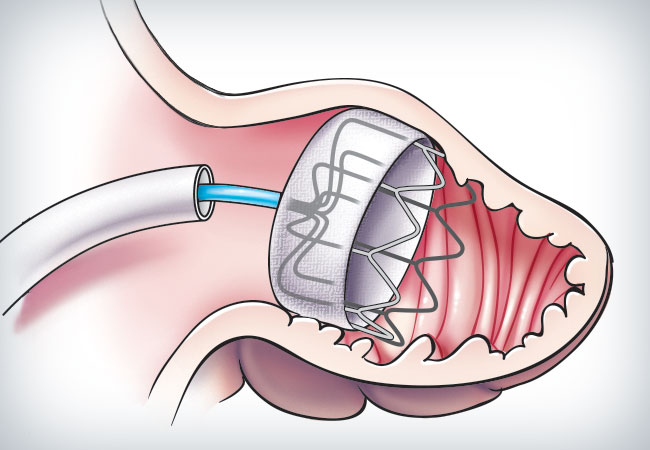
We will be talking today about left atrial appendage closure in the setting of atrial fibrillation in patients who cannot tolerate oral anticoagulation. Now, Dr. Kanj, who is our co-director of the EP lab, could you tell us if we are able to do a left atrial appendage closure at the time of atrial fibrillation ablation and who is the ideal patient for this procedure?
Mohamed Kanj, MD:
This is an excellent question. I mean, it's not uncommon that we have patients who may need atrial fibrillation ablation, but at the same time, they have some concerns about taking oral anticoagulation or vice versa, especially that we know the procedure where we close the left atrial appendage is technically, shares a lot of the steps with an ablation procedure.
Mohamed Kanj, MD:
So here at the Cleveland Clinic, we've had a good experience so far with doing concomitant procedures. We've been doing that for the past almost six years, and we've had our great track records with excellent safety and efficacy of both of these procedures being done at the same time. I think we are probably the few centers, if not the biggest center in the US, who perform both procedures at the same time.
Mohamed Kanj, MD:
The advantage is, is patients could have both things done in one visit, the ablation at the same time as closing the left atrial appendage. In this way, we hope that for the patients taking care of the atrial fibrillation, but at the same time, being able to come off oral anticoagulation after two to three month after doing the concomitant procedure.
Oussama Wazni, MD, MBA:
Could you tell us about how many we've done so far?
Mohamed Kanj, MD:
We have done around 300-plus patients, and so far, some of these patients, in 150 of them, we've had more than a year good, excellent follow-up with very, very low complication rate. We did not see that doing both procedure would increase their complication rate significantly, but we're getting, in fact, good results, excellent results.
Oussama Wazni, MD, MBA:
I think this is the highest single-center experience in the world. I mean, there are some pooled data from other places, but I don't think that a single center has been able to achieve this number. So that's a great testament to the teamwork that we do here at the Clinic because this also involves a clinical cardiologist, an imaging cardiologist, their own patient's physician and our team here at the Cleveland Clinic.
Oussama Wazni, MD, MBA:
We're going to switch gears here now and with Dr. Tyler Taigen, who is our director of the outpatient department, and also the director of our quality control here at the Clinic that we take very seriously. Dr. Taigen, a lot of our patients are not simple. They have complex issues and have had previous procedures in the past. Can left atrial appendage closures be performed in patients, I'll give you a few scenarios here, a patient who's had valve surgery, mitral or aortic valve surgery, a patient who has a atrial septal defect, for example, closure device? Can left atrial appendage closure be performed in these patients? Are there any restrictions?
Tyler Taigen, MD:
Yeah, that's a great question. I think the way you approach this is to step back and think about AFib in general, when we use anticoagulants, how we approach stroke prevention, just in general terms. In some ways, this isn't that different than looking at direct oral anticoagulants versus warfarin. Warfarin has got a much broader indication. A lot of this comes down to whether or not we think this is non-valvular AFib, and that can get confusing. I think people look at that and think that a little bit of regurgitation or stenosis, or even a prior surgery, may be a contraindication to either direct oral anticoagulant or potentially closing the left atrial appendage. Although that hasn't been studied clearly, it is the case that direct oral anticoagulants and the Watchman or other forms of closing the appendage are safe in that situation. We've had that.
Tyler Taigen, MD:
Valvular heart disease is when someone has a mechanical valve, has rheumatic heart disease, significant stenosis. That's a different population. If someone needs to be on a blood thinner for some other reason, and warfarin is better, then that's a different population. But for these patients that we see quite a few of here that have complex disease, that had closures or complicated valve surgeries with bioprosthetic valves and an open appendage, the answer is that we have done those. The outcomes are good. I've looked at the quality and it's similar to what we see with patients that don't have that.
Tyler Taigen, MD:
Specifically with the ASD, there is a warning because it can be difficult to get around the ASD. But if the imaging is good, we have been successful at getting transeptal access around the ASD and then implanting a Watchman device in the left atrial appendage, closing it, and then getting the patient off the blood thinner.
Walid Saliba, MD:
Just to extrapolate that, how about patients who have had percutaneous valve procedures like TAVR and mitral clip and tricuspid valves clip? Is there a problem, consideration to putting a left atrial appendage closure device in these patients if they are candidate for it?
Tyler Taigen, MD:
Yeah. I think it's the same thing that we don't have a lot of trial evidence in this group and it's growing. But places where we're innovating and looking at this, we can do it. I think it is safe and our outcomes have been as good in that group as they have been and those that haven't had those procedures.
Oussama Wazni, MD, MBA:
Finally, we want to address the issue of leaks and this is going to be for the three of you here and what do we do about leaks? When is a leak important? Because I know now a lot of patients may have already had left atrial appendage closure and now they go back for follow-up and they're told, "Sorry, but there is a leak and we may need to do something about the leak." So I'm going to start with Dr. Saliba here. Could you tell us what the data supposedly says about leaks? When are they important? Are they important at all? Then we'll move down the panel and talk about what are the options, if we think that the leak is important or significant that we need to do something about it.
Walid Saliba, MD:
That is an important question. I will tell you what we know now and what do we do now and I can just give you a brief idea about where we think this is going. When we put a device, obviously, the idea is for the device to seal the opening of the left atrial appendage so we do not want to see any leaks around that device. When we looked at the data of how many of these devices that were placed do have a leak, well, with the newer devices, I would say probably around 10% or so will show some kind of a leak. Not bad leaks and when I say not bad leaks, meaning that the size of the leak from around the device is less than 5 millimeter and that is, let's say, an arbitrary kind of measurement. Less than 10.5% of the patients have a certain amount of leak. Now, the question is, if you have more than 5 millimeter leak, then that is an issue and those patients, we have to continue oral anticoagulation because with that size of a leak, then probably the seal is not great and the risk of stroke is as bad as if you don't have the device.
Walid Saliba, MD:
But if the leak is less than 5 millimeter, what we originally knew is that it is okay not to restart oral anticoagulation because the risk is not significantly high. But there is now new data emerging with longer term follow-up that seems to suggest that if there is a leak, then the risk is slightly higher than if you don't have a leak. And those patients, what do we do with them? Do we continue oral anticoagulation? Do we try to close the leak in some certain ways? Or do we say, "It's okay, the leak is small. Let's just keep them off anticoagulation?" This is where the research is now trying to answer those questions that we have. This is work in progress and this is a very dynamic field at this point in time.
Oussama Wazni, MD, MBA:
This is very important because we have a large study led by Dr. Saliba now. It's called the Real World Evidence in Watchman. This is pertaining mostly to Watchman so that we can... Pardon me? Watchman FLX to look at leaks and other things also, but this will be one of the important aspects to look at. Now, I'll just say quickly, before I turn it to Dr. Kanj and Dr. Tyler, no, Dr. Taigen in that here at the Clinic, we make sure that nobody goes out with a leak. That's the most important aspect. We take our time and we make sure that the original implant has no leak because going out with a small leak may end up becoming a big leak. So the most important thing for our patients and actually for our referring physicians to know is that we take as much time as needed. Especially with the new devices, we can reposition multiple times to get the ideal positioning and ideal result with no leaks.
Oussama Wazni, MD, MBA:
Now, suppose still, we have somebody who ends up with a leak and by the way, the data that Dr. Saliba was talking about is not our own data, this is from the previous studies and also from registry data. But now we have a patient who does have a leak. They got their device elsewhere and they have a significant leak. Are there options that we can give this patient, Dr. Kanj?
Mohamed Kanj, MD:
Yes. The disclaimer is that yes, we know that these leaks do matter, but we want to make sure that although they do matter, patients will still get benefit from having the device in. So it's not that it's going to put the patient at any increased risk. It's that is the benefit is less if you have a leak compared to you don't have a leak. So they still have significant benefit even if there's a little bit of a leak around the device.
Mohamed Kanj, MD:
What to do with that? You know, this is a field of research right now, but most of us think that if it is a significant leak, we could offer to the patient after a careful shared decision-making the possibility of closing this leak. Depending on the shape, because the leak is a two-dimensional shape and it's most of the time like a crescent, depending on the size of the crescent and where's the location, we may offer a few things. For example, sometimes we could put a vascular plug, sometimes you could consider an Amplatzer plug and sometimes you could consider coiling or sometimes you could consider the combination of all these therapies. Again, the disclaimer is that we don't know that efficacy of all of these strategies, but theoretically, they may offer some benefit.
Oussama Wazni, MD, MBA:
Thank you. Thank you, Doc.
Oussama Wazni, MD, MBA:
Then finally for Dr. Taigen, now we've had a few cases where it's not a small leak. It was a big leak or a device that had moved and that is a possibility and we recently had a patient like that. So could we speak to that and what are the options there and what we can do?
Tyler Taigen, MD:
If the device moves and that doesn't necessarily mean that it's freely embolizing and moving around in the left atrium, it could just be that it's rocked out and it's moving back and forth and has obviously lost its hold. Many times when that's happened, then it's going to require surgical backup, which is what we ended up doing on the patient that came in. I think the important point on this, though, is with that initial implant, I think especially if it's one of these that is trabeculated with large pectinate, to not leave leaks at the start and not have those big shoulders, in particular with any kind of leak, because those are the ones that I think are higher risk. These, fortunately, after doing thousands here, we really haven't seen that much of this at all with it.
Oussama Wazni, MD, MBA:
No, we have not.
Tyler Taigen, MD:
What's more common, I think, is a small leak that they can come after that's a millimeter or two, like Dr. Saliba mentioned. Then my practice on that would often be to leave them on the blood thinner for a little bit longer, image again in three months and the majority of those for all of us, they're gone at that point. So I think that's how you handle this. I'm not sure if it's clinically significant and those tend to get better.
Oussama Wazni, MD, MBA:
In our situation here, because we are at the Cleveland Clinic, we have fantastic surgeon colleagues who, although we get the call about those devices and their misplacement or displacement, we are able to lean on them to provide the excellent care to our patients. So this patient who, again was implanted elsewhere, but had a displaced device, was able to get surgery to remove the device, close the appendage and actually also get a Maze procedure for her atrial fibrillation that continued to be symptomatic and she's doing very well at this moment.
Oussama Wazni, MD, MBA:
On that good note, I want to thank you all for your participation. I just want to remind our listeners and the physicians on the podcast that the indication for left atrial appendage closure now is somebody who has atrial fibrillation, an indication for prevention of stroke because of a high CHA2DS2-VASc Score and we defined that earlier in the podcast, but they can't be on blood thinners because of bleeding issues. Then it's a good indication to close that appendage, provided they do not have valvular atrial fibrillation, which we also defined, and that's a mechanical valve or rheumatic heart disease with a stenotic mitral valve and then we're able to manage those patients. Even if they had an ASD closure device, we're able to maneuver around it. Even if they've had, for example, a TAVR or a MitraClip. Actually one of our, our chairman, Dr. Kapadia, is leading the study on TAVR plus Watchman together. It's called the Watch-TAVR Study. Then also on the concomitant side, we have a big study that we finished enrolling in called the Option Trial. It's about AFib ablation and left atrial appendage closure and a lot of those patients, up to 40% of them, are getting the ablation plus Watchman FLX in the same setting. I think the future for left atrial appendage closure and stroke prevention is very good and before we completely close, we'll ask if there are any other comments from the panelist.
Walid Saliba, MD:
I just want to expand on what Dr. Wazni said that we also have research now in patients who are allowed to be on oral anticoagulation, but the research, the study actually take those patients and randomizes them 50-50, left atrial appendage closure versus continuation of oral anticoagulation, to see if left atrial appendage closure is beneficial as an alternative option to oral anticoagulation in patients who do not have problems bleeding who can take oral anticoagulation. So this is an attempt to expand the indication for left atrial appendage closure and this is research that is on the way at the Clinic at this point.
Oussama Wazni, MD, MBA:
That's an important one. Thank you, Dr. Saliba. Again, these studies, there are two of them. One is called Champion and the other one is called Catalyst and this is in patients who do not have bleeding issues. But again, this is research now and the patients will be randomized to continue blood thinners or get a device. If you're interested, please contact us. We are still looking for patients, we are still recruiting. These are very large studies, more than 3,000 patients in each of those studies, but it will allow us and provide us a lot of information on whether one day we can replace oral anticoagulants altogether with a device.
Oussama Wazni, MD, MBA:
Of course, that is not the message right now. Right now, the message is left atrial appendage closure is a good alternative to blood thinners in people having bleeding problems. Thank you once more for your attention and we look forward to seeing you in the next podcast from Cleveland Clinic Electrophysiology. Thank you.
Announcer:
Thank you for listening. We hope you enjoyed the podcast. We welcome your comments and feedback. Please contact us at heart@ccf.org. Like what you heard? Subscribe wherever you get your podcasts or listen at clevelandclinic.org/cardiacconsultpodcast.

Cardiac Consult
A Cleveland Clinic podcast exploring heart, vascular and thoracic topics of interest to healthcare providers: medical and surgical treatments, diagnostic testing, medical conditions, and research, technology and practice issues.



