A hysterectomy is a surgical procedure that removes your uterus. After surgery, you can’t become pregnant and won’t get a menstrual period. Reasons for this surgery include abnormal bleeding, uterine prolapse, fibroids and cancer. Recovery usually takes four to six weeks, depending on the type of surgery you have.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
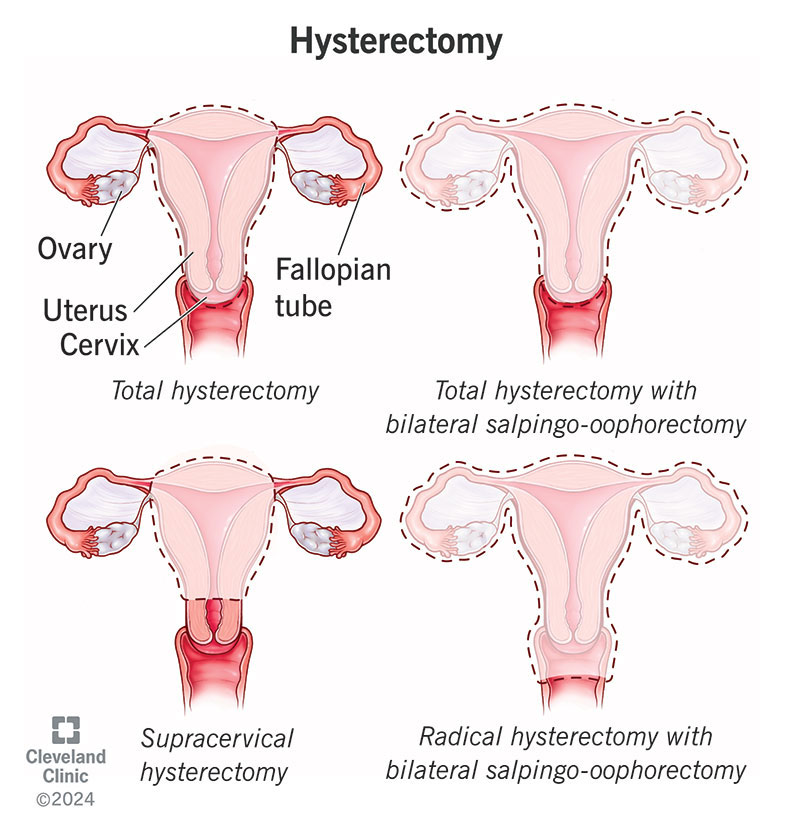
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4852-hysterectomy)
A hysterectomy is the surgical removal of your uterus and, most likely, your cervix. Depending on the reason for the surgery, a hysterectomy may involve removing surrounding organs and tissues, like your fallopian tubes and ovaries.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You won’t be able to get pregnant and you won’t get your menstrual period after a hysterectomy.
Your healthcare provider will discuss which type of hysterectomy you need, depending on your condition. This will determine if they’ll also need to remove your fallopian tubes and/or ovaries.
The different types of hysterectomy surgeries are:
Advertisement
Healthcare providers often suggest alternative treatments before recommending a hysterectomy. This mostly depends on the reason for needing a hysterectomy. Sometimes, those treatments don’t help, or surgery is the only option to treat the condition.
Surgeons perform hysterectomies to treat:
Many people have a hysterectomy to prevent cancer. For people at high risk for certain types of cancer, removing the uterus (and/or surrounding reproductive organs) can reduce the chances of developing cancer.
Approximately 600,000 females get hysterectomies in the United States each year.
A healthcare provider will explain the procedure in detail, including possible complications and side effects. Talk to them about any concerns you have about the surgery and the recovery process. You may need to provide blood and urine samples to make sure you’re healthy enough for surgery.
A hysterectomy may not involve a hospital stay, depending on what type you have and the surgical approach your surgeon uses. Be sure to discuss what support you’ll need in the early days of your recovery so you can plan for help.
Your healthcare provider will determine the type of hysterectomy you need and the best surgical method to perform that procedure. You’ll change into a hospital gown and get hooked up to monitors that track your heart rate. A healthcare provider will place an intravenous (IV) line in a vein in your arm to deliver medications and fluids.
An anesthesiologist will give you either:
There are several different surgical approaches your healthcare provider may use to perform a hysterectomy.
Advertisement
Advertisement
The procedure lasts one to three hours. The time can vary depending on:
Anesthesia will keep you from feeling pain during the surgery. But you can expect soreness and discomfort for a few weeks. Your surgeon will discuss your options for pain relief during recovery. This could involve prescription pain medication or over-the-counter (OTC) pain medicines like NSAIDs (non-steroidal anti-inflammatory drugs) or acetaminophen.
Some of the most common side effects of a hysterectomy are:
Advertisement
If your healthcare provider removes your ovaries at the time of your hysterectomy, and you haven’t already gone through menopause, you may experience symptoms of menopause, such as:
Your surgeon will discuss treatment options to avoid the side effects of menopause if they remove your ovaries. This could include hormone replacement therapy (HRT) to relieve your symptoms.
The amount of time you spend in the hospital following a hysterectomy varies depending on what kind of surgery you had. Your healthcare provider may want to monitor you and ensure there aren’t any signs of complications. You’ll walk around as soon as possible after your surgery to prevent blood clots in your legs.
If you had an abdominal hysterectomy, you might stay in the hospital for a few days. Vaginal and laparoscopic hysterectomies are less invasive and typically don’t require an overnight stay in the hospital.
Your healthcare provider will go over recovery instructions, including restrictions to your day-to-day activities. Be sure to discuss any concerns you have about your recovery or the procedure before you go home.
You typically don’t need to be on bed rest after a hysterectomy. In fact, your provider will want you to walk around as soon as you’re able to.
The types of changes you can expect to your body depend on what kind of hysterectomy you have. If your provider removes your ovaries, you can expect to enter menopause right away. In addition to the usual side effects of surgery, you may also have symptoms of menopause. Talk to your healthcare provider about ways to minimize symptoms of menopause.
If your provider keeps your ovaries, you won’t enter menopause. In this case, you’ll still lose the ability to get pregnant, but your ovaries will continue to make hormones. You’ll enter menopause at a more typical age (around 51).
As with any major surgery, recovery and rest is crucial. Allow yourself time to heal. Your body has been through a lot, so prioritize rest and relaxation for at least the first two weeks.
Having a hysterectomy can help you live a more enjoyable life, especially if you have constant pelvic pain or heavy and irregular bleeding. If you’re at a higher risk of uterine cancer, a hysterectomy can lower this risk. Having your cervix removed means you may not need pap smears any longer. Having your fallopian tubes removed reduces the risk of ovarian cancer even if your ovaries aren’t removed.
A hysterectomy is a major surgery with a long recovery. It comes with risks and side effects and is permanent. Depending on the type of surgery you have, you can go into menopause or experience symptoms of menopause immediately after. You also won’t be able to become pregnant after any type of hysterectomy.
As with any surgery, there’s a slight chance that problems may occur, including:
Most people recover from a hysterectomy in about four to six weeks. Your recovery depends on the type of hysterectomy you had and the method your surgeon used. Recovering from a vaginal and laparoscopic hysterectomy takes less time than recovering from an abdominal hysterectomy.
You should increase your activity gradually and pay attention to how you feel. If anything causes you pain, you should stop. Talk to your healthcare provider about specific instructions for recovering at home, including what medications to take.
Vaginal and laparoscopic recoveries take about two to four weeks. It may take up to six weeks to recover from abdominal hysterectomy. In most cases, you’ll receive papers with instructions that specify what activities you can and can’t do and for how long.
Talk to your healthcare provider before going home to make sure you know how to best care for yourself.
Some things you can expect after surgery include:
It’s normal to feel slightly different physically and emotionally after a hysterectomy, especially during your recovery.
After a hysterectomy, your periods will stop. Occasionally, you may feel bloated and have symptoms similar to when you were menstruating.
You may feel discomfort at abdominal incision sites for about four weeks, and any redness, bruising or swelling will disappear in four to six weeks. Feeling burning or itching around the incisions is normal. You may also experience a numb feeling around the incisions or down your leg. This is normal and, if present, usually lasts about two months.
It’s normal to have scarring from the surgery, both internally and externally. Abdominal laparoscopic surgeries will cause smaller, less visible scars as opposed to abdominal hysterectomies, which will be larger.
People who undergo supracervical hysterectomy may continue to have light periods for a year after the procedure. This happens because small amounts of the endometrial lining can remain in your cervix, causing light periods.
Emotional reactions to a hysterectomy vary and can depend on how well you were mentally prepared for the surgery and the reason for having it.
You may feel a sense of loss, but these emotional reactions are usually temporary. Others may find that a hysterectomy improves their health and well-being and may even be a life-saving operation. Please discuss your emotional concerns with your healthcare provider and see if they recommend counseling or a support group to help you cope.
This depends on if your surgeon removed your cervix and why you had the hysterectomy. If you still have a cervix, you should continue to get Pap smears to screen for cervical cancer. If you don’t have a cervix, you may not need a Pap test.
Call your healthcare provider if you have:
A hysterectomy shouldn’t affect your sexual function. If you enter menopause as a result of a hysterectomy, you could have symptoms like low sex drive and vaginal dryness. Let your healthcare provider know if you experience uncomfortable side effects of menopause so they can recommend a treatment.
After you have a hysterectomy, your other organs move to fill the space. Your small and large intestines mainly fill the space once occupied by your uterus.
Your healthcare provider will work with you to develop the best treatment plan for your symptoms or condition. When a hysterectomy isn’t medically necessary, some alternatives to try could be:
Sitting on the toilet after a hysterectomy may be a little uncomfortable, especially if you had an abdominal hysterectomy. Supporting your belly and abdomen can help you feel a little better when you sit down. It may feel a little better to lean forward into a pillow when you sit on the toilet. This may take pressure off your abdomen (it takes more work to sit up straight).
Some people find squatting to be painful, so if you can adjust your toilet to be higher, that could be an option. If you can’t do this, sit down slowly and gently while you try to position yourself.
It’s very normal to experience bloating or gassiness after a hysterectomy. It can take several weeks for the puffiness and swelling in your belly to go down. Talk to your healthcare provider about ways to reduce your discomfort. Performing certain exercises and applying a warm compress may help.
Getting a hysterectomy can be an emotional experience. While it can offer relief and peace of mind, it can also be a difficult recovery and leave you with feelings of loss. If your healthcare provider recommends a hysterectomy, make sure you understand the procedure and how to safely recover from surgery. Be sure to follow their recommendations on things to avoid while you recover at home. Most people can go back to their usual activities six to eight weeks after a hysterectomy.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s gynecologic providers do all types of hysterectomies. We explain your treatment options so you can make an informed decision about your care.
