If you have to remove your whole colon due to a serious disease, you’ll need an alternative route to pass poop from your body. The J-pouch is one solution that your surgeon can create. It’s an internal pouch made from the end of your small intestine that connects to your anal canal. This allows you to poop on a toilet in the old-fashioned way.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
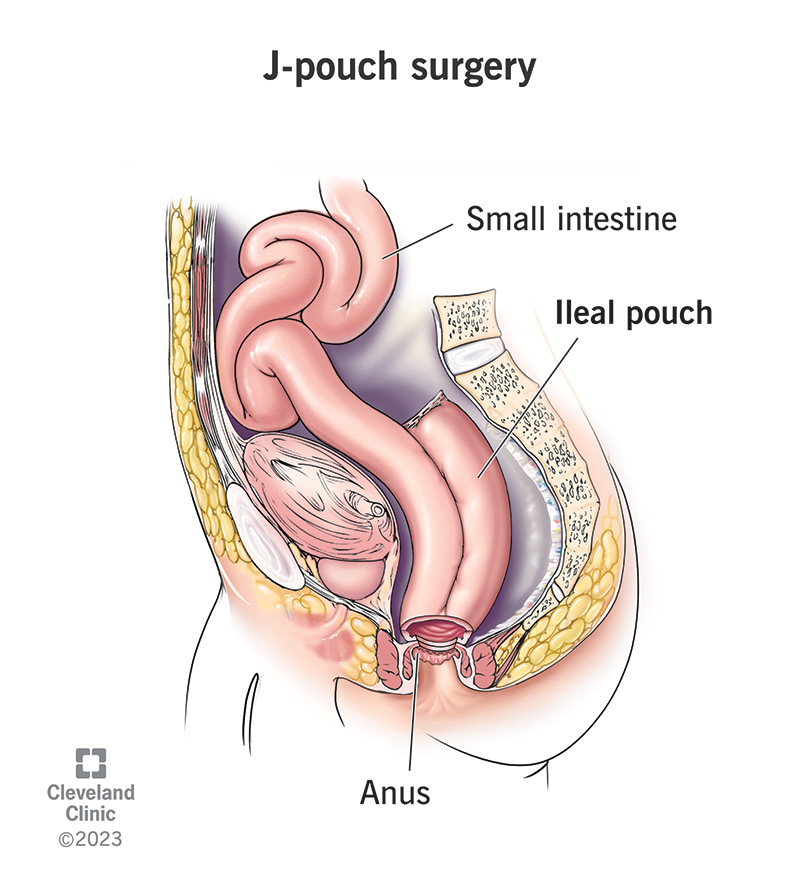
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21062-j-pouch-surgery)
A J-pouch is one type of ileal pouch that a surgeon can create inside your body to replace your colon and rectum. A surgeon constructs an ileal pouch from your ileum, which is the end of your small intestine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are a few different types of ileal pouches, but the J-pouch is the most popular one today. The pouch acts as a reservoir for your poop that connects to your anus (butthole), the way your rectum once did.
If you’ve had or need to have a total proctocolectomy, you may wish to have a J-pouch with it. A total proctocolectomy removes your colon and rectum when they’ve become unusable due to disease.
When most of your large intestine is gone, you’ll need an alternative way to pass food waste (poop) from your body. J-pouch surgery is one solution that allows you to continue to poop through your anus.
The J-pouch is an alternative to a permanent ileostomy. If your anus is still functional, the J-pouch can replace your colon and rectum internally. It reconnects your ileum and anus so you can poop normally.
An ileostomy, on the other hand, diverts your ileum to a new opening in your abdomen called a stoma. Your poop comes out of the stoma into an external ileostomy bag, which you’ll then empty.
The J-pouch is an internal pouch that mimics your original anatomy. It empties itself through your anus as your rectum used to do. When it’s full, you’ll feel the urge to poop and find a bathroom.
Advertisement
You may be a candidate for J-pouch surgery after your proctocolectomy if:
Your surgeon will discuss these factors with you before and after your proctocolectomy.
J-pouch surgery usually happens in two to three stages, beginning with your total proctocolectomy. Your surgeon may begin the process during your proctocolectomy surgery or later in a separate surgery.
You’ll have a temporary ileostomy after your proctocolectomy unless you’re having a permanent ileostomy instead. Your temporary ileostomy will remain until your J-pouch is ready to use.
Your surgeon will:
After the procedure, your body will need time to adapt to your new anatomy. Your J-pouch will be small at first, with little capacity. It’ll gradually stretch out over the following months as you use it more.
This means you won’t be able to hold much poop in the beginning. You’ll probably poop more often during the day and a few times during the night. This will gradually improve over time.
In addition, your anal muscles will be weak from a lack of exercise. You may need to retrain them to control your bowel movements. Your provider might suggest Kegel exercises to help with this.
Your healthcare provider will be there to support your recovery process. They’ll continue to monitor your condition and look for signs of possible complications during follow-up appointments.
Risks of J-pouch surgery include:
Advertisement
J-pouch complications include:
Advertisement
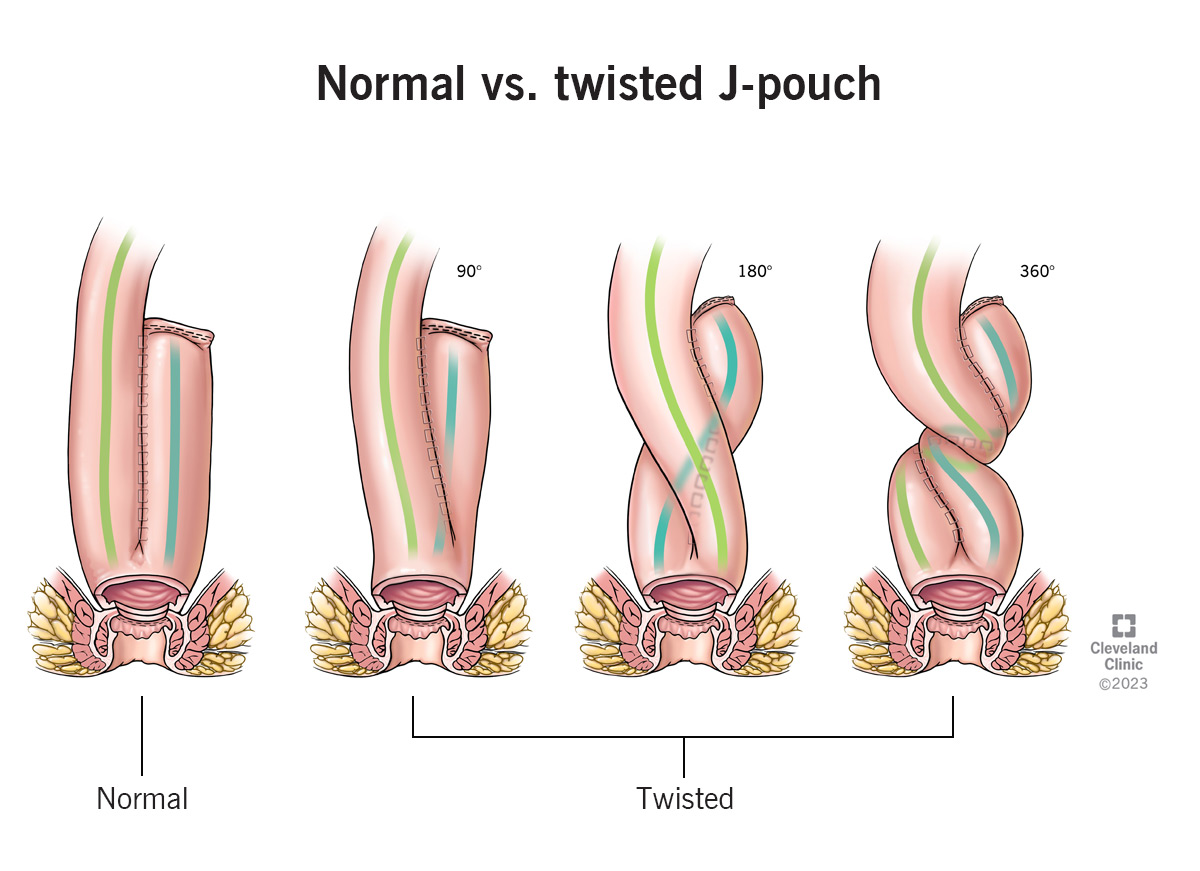
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/21062-j-pouch-surgery-2.jpg)
In twisted pouch syndrome, your J-pouch is rotated in your pelvis at the time of construction.
The estimated long-term success rate is 95%. A small number of J-pouches fail. Failure means the pouch has persistent complications that prevent it from working well, and it needs to be removed or replaced. In this case, your quality of life is better with a good permanent ileostomy than with a bad ileal pouch.
J-pouch failure is possible when you’ve had troublesome symptoms for a long time that persist despite treatment. These will usually be symptoms of inflammation in or around your pouch, like:
When you have a total proctocolectomy, the way you poop will change forever. Whether this is an elective surgery or a lifesaving one, it helps to know that you’ll have some options going forward.
Your choice will be either to have a permanent ileostomy or an internal ileal-anal pouch. For most people, this means the J-pouch. (Other ileal pouches are used in special circumstances.)
The J-pouch is a simple and effective design. It connects to your anus, allowing you to poop using normal pooping muscles and nerves. It holds your poop until it’s ready to come out, like a new rectum.
Advertisement
The J-pouch eliminates the need to live with and care for a stoma and an ostomy bag. While you’ll poop more often than before, you’ll maintain bodily control over when and where you poop.
You’ll use the bathroom normally with a J-pouch, although it’ll be more often than before. You may have more than 10 bowel movements a day at first, then settle down to between five and 10.
Your poop will also be wetter because it’s traveling a much shorter distance than before. Without passing through your colon, your poop won’t have the chance to slowly solidify as it used to.
This also means that your body won’t be able to reabsorb fluids from your poop as it used to. You’ll need to take extra care to stay hydrated. However, this is also true with an ileostomy.
Most people report an improved quality of life after J-pouch surgery. You’re free of the disease that caused you to have a total proctocolectomy, and you’re also free of the demands of an ileostomy.
There’s no one prescribed diet for people living with a J-pouch. But eating a balanced, healthy diet will help you heal well and avoid bothersome symptoms. Your healthcare providers might suggest:
J-pouch surgery is a big step, and it’s natural to feel nervous about how it’ll change your life. Take all the time you need to research and ask questions about the procedure before you take the leap.
When you’re ready, don’t forget to reach out to your social support system. It helps to have a dedicated friend or family member to accompany you to the hospital and help you manage after your surgeries.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Having your colon removed can change your life. Our J-pouch surgery experts will help you keep things as normal as possible moving forward.
