Inflammatory bowel disease (IBD) includes Crohn’s disease and ulcerative colitis. IBD causes symptoms like belly pain and cramps, diarrhea and blood in your poop (stool). Inflammatory bowel disease is chronic and can’t be cured. There are treatments that can put the disease into remission but IBD often comes back.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
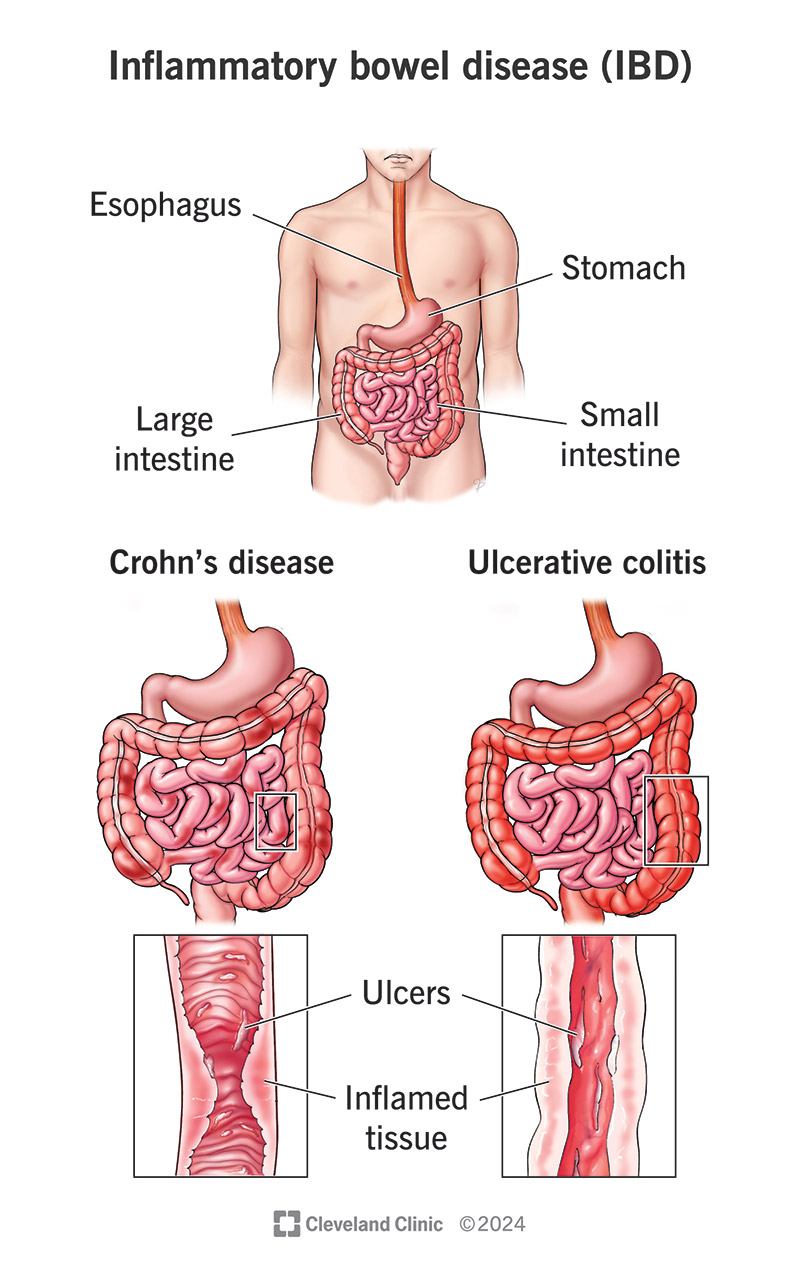
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/15587-inflammatory-bowel-disease-ibd.jpg)
Inflammatory bowel disease (IBD) refers to diseases that cause chronic inflammation in your gastrointestinal (GI) tract. Its symptoms may come on suddenly (flares) and cause intense stomach cramps and diarrhea, among other issues. But IBD can affect more than your gut — it can affect your overall physical health, emotional well-being and even your mental health.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Inflammatory bowel disease is a lifelong illness for which there’s no cure. This may sound grim. But there are treatments that manage IBD symptoms, and steps you can take to keep IBD from disrupting your life.
Crohn’s disease and ulcerative colitis are the main types of IBD:
Experts estimate that 1.6 million people in the U.S. have IBD. The disease can affect anyone from young children to adults age 65 and older. But it most commonly affects people ages 15 to 35.
IBD symptoms may be mild or severe. They come and go, and you can’t always predict when they’ll happen. When they do, a healthcare provider may say you’re having an IBD flare (active disease). When your symptoms go away after treatment, a provider may say the disease is in remission. Common IBD symptoms include:
Advertisement
IBD happens when immune system cells in your GI tract mistakenly attack healthy tissue, causing inflammation that leads to Crohn’s disease and ulcerative colitis. Researchers don’t know the exact reason why this happens. But they’re studying mutations in certain genes that normally:
When these genes mutate (change), it increases your risk of IBD. Researchers may call these genes susceptibility genes. There are more than 160 different susceptibility genes. If you inherited any number of them, several everyday activities could trigger IBD symptoms. These activities don’t cause the disease. Common IBD triggers include:
Researchers are also investigating if issues with your gut microbiome may play a part in the chronic inflammation that causes IBD.
No, but you may notice that your symptoms get worse after you consume certain foods or liquids. Everyone is different, but food and drink that may make you feel worse may include:
The most significant risk is having a family history of IBD. Studies show that 5% to 20% of people with IBD have a close family member — parent, sibling or child — who has IBD.
IBD may cause other medical conditions in your GI tract and beyond. Some may be medical emergencies or serious illnesses, including:
Other IBD complications that affect your GI tract are anal fistula and anal stenosis. Anal stenosis is when your anal canal narrows, making it hard for poop to leave your body.
IBD may increase your risk of complications like:
Advertisement
A healthcare provider will do a physical examination. They’ll ask about your symptoms, including how long you’ve had them, if your symptoms are mild or severe and if they come and go. They may order the following tests:
Treatments vary depending on the type of IBD that you have, but all treatments focus on bringing IBD into remission — and keeping it there. A healthcare provider may prescribe medication to ease symptoms. In some cases, you may need surgery if medications aren’t effective.
In general, medications for IBD focus on managing inflammation and controlling your immune system’s response. Healthcare providers may use the same types of prescription medication to treat Crohn’s disease and ulcerative colitis. Medications may include:
Advertisement
IBD medication may manage your symptoms for many years. But if medications stop working, your provider may recommend surgeries like a colectomy.
IBD is a chronic condition that you’ll need to manage for the rest of your life. Having this condition also increases your risk of serious illnesses like colon cancer.
For those reasons, you should plan on regular visits to your healthcare provider even when you don’t have symptoms. Your provider may recommend you schedule appointments every six months when IBD is in remission, and more often when you have an IBD flare. If you’re in your 30s or 40s, your provider may recommend you start receiving routine colonoscopies earlier than most people.
It’s not always easy to live with IBD. Symptoms may flare up and then go away for weeks and months. You may find yourself wondering when the next flare will hit. You may feel embarrassed or self-conscious about symptoms like sudden bouts of diarrhea that make you race for the bathroom. Here are some suggestions that may help you manage IBD:
Advertisement
Medication and self-care often help keep IBS in remission. But you should contact your healthcare provider if you have IBS flares that don’t go away.
If you have IBD, you have an increased risk of conditions like toxic megacolon or perforated bowel that are medical emergencies. Call 911 (or your local emergency service number) or go to the emergency room if you have the following symptoms:
Both IBD and IBS affect your gut. The difference is that IBD involves inflammation, but IBS doesn’t.
If your diagnosis is inflammatory bowel disease, you may be relieved to know why you have a crampy belly and diarrhea for days on end. And it probably helps to know how treatment can make your symptoms go away. But you may worry about what it means to have a chronic disease with uncomfortable and sometimes embarrassing symptoms that may happen without warning. Your healthcare providers know that IBD can disrupt your daily routine. They’ll have suggestions for managing your symptoms and living well with IBD.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
You don’t have to let inflammatory bowel disease control your life. Cleveland Clinic is here to help you feel like yourself again.
