Pulmonary fibrosis is scarring in your lungs. It can make it hard to expand your lungs and get enough oxygen to your body. It can be idiopathic (without a known cause) or result from autoimmune diseases, environmental factors or medications. Pulmonary fibrosis usually gets worse over time, but how quickly it gets worse is different for everyone.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
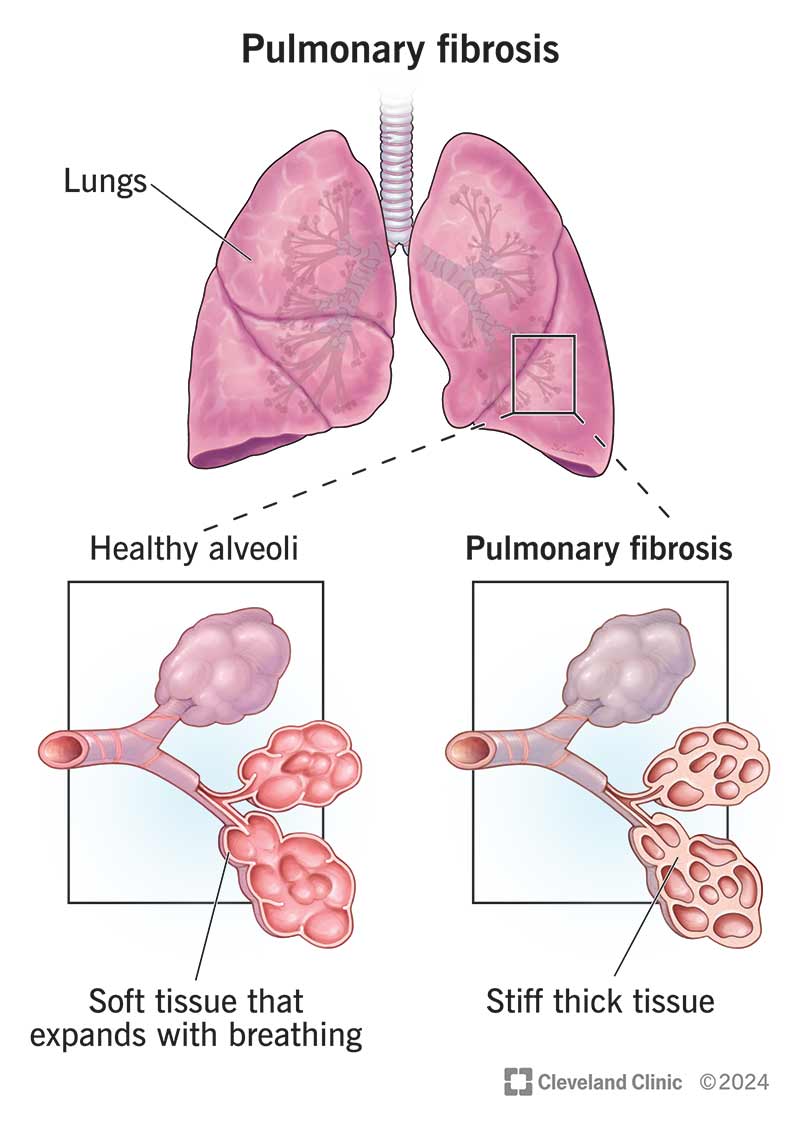
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/pulmonary-fibrosis)
Pulmonary fibrosis (PF) is a scarring and thickening in your lungs that makes it hard to breathe deeply. It’s a type of interstitial lung disease, which affects the tissue between the air sacs in your lungs (alveoli).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hard, stiff lung tissues don’t expand as well as they should. If you have pulmonary fibrosis, you may get short of breath during daily tasks that never seemed tiring before. Pulmonary fibrosis is permanent and usually gets progressively worse over time (called progressive pulmonary fibrosis).
Idiopathic pulmonary fibrosis is lung scarring without a known cause. Most cases of pulmonary fibrosis are idiopathic.
Pulmonary fibrosis symptoms include:
Experts think pulmonary fibrosis happens when your lungs don’t heal properly from damage or inflammation. Specific causes include:
Advertisement
In most cases, the specific cause is unknown.
In addition to the causes above, you might also be at a higher risk for pulmonary fibrosis if you:
Scarred lung tissues have a hard time getting oxygen to the rest of your body and can make your heart work harder. This can lead to complications that include:
It might take a number of tests and imaging procedures to diagnose pulmonary fibrosis. Your provider will listen to your lungs and get pulmonary function tests to understand how your lungs are working. They’ll check for and rule out other conditions that affect your heart and lungs.
Specific tests and procedures providers might use to diagnose pulmonary fibrosis include:
They may also use an echocardiogram to diagnose or rule out issues with your heart.
No, there isn’t a cure for pulmonary fibrosis. Treatment focuses on easing symptoms, slowing down progression, and improving your quality of life.
Treatments for pulmonary fibrosis could include:
You may also need medications to treat underlying causes (like autoimmune disease) or conditions that make scarring worse (like GERD).
If you have a PF diagnosis, it might be harder to fight off or recover from infections. Washing your hands frequently, disinfecting surfaces and avoiding crowded places — especially during cold and flu season, and when COVID-19 cases are high — might help you avoid getting sick frequently. Getting recommended vaccinations, like those for pneumonia, the flu, RSV, and COVID can also help minimize your risk.
Advertisement
Talk to a healthcare provider if you have shortness of breath or get tired more easily with everyday tasks than you used to. Early diagnosis and treatment can help slow down the progression of lung disease.
If you have a connective tissue or granulomatous disease, talk to your healthcare provider about whether there are ways to reduce your risk of fibrosis.
Call 911 or go to the emergency room if you experience:
It might be helpful to ask your healthcare provider:
Lung scarring is nearly always permanent (unless caused by a medication and caught early). If you have an underlying disease, management of it might help prevent further damage. If the cause is unknown, your healthcare provider will treat your symptoms and try to prevent more damage.
Healthcare providers can’t easily predict how pulmonary fibrosis will progress. Your symptoms may get worse very slowly, over years. In some cases, the disease may lead to severe symptoms quickly (over months).
Advertisement
The life expectancy of someone with the most common form, idiopathic pulmonary fibrosis, is three to five years. But life expectancies for people with PF have been getting longer in recent years.
Many causes of pulmonary fibrosis aren’t preventable. You can reduce your risk of lung scarring from environmental exposures by:
While there’s no official staging system for pulmonary fibrosis, some providers may describe pulmonary fibrosis as mild, moderate, severe or very severe. They base this diagnosis on your symptoms, lung function tests and imaging.
Most cases of pulmonary fibrosis are diagnosed in people 65 and older.
Finding out you have pulmonary fibrosis can be life-changing. You might feel uncertain about your future, or like the rug’s been pulled out from under you. Finding a support system in loved ones or in others with the same diagnosis can help.
Advertisement
It’s important to remember that every case of PF is different, and no one can tell you what your future holds. Treatment can sometimes slow down the progression of pulmonary fibrosis and improve your quality of life. Have honest conversations with your provider about what you can expect in your specific situation.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Breathing issues can affect your life in many ways. Cleveland Clinic’s respiratory therapy program treats your symptoms so you can feel better day to day.
