Familial Mediterranean fever (FMF) causes episodes of fever and inflammation in your belly, chest and joints. It usually affects people with Mediterranean or Middle Eastern ethnic backgrounds. Colchicine is the most common medication to treat FMF. It can help you have fewer episodes and milder symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
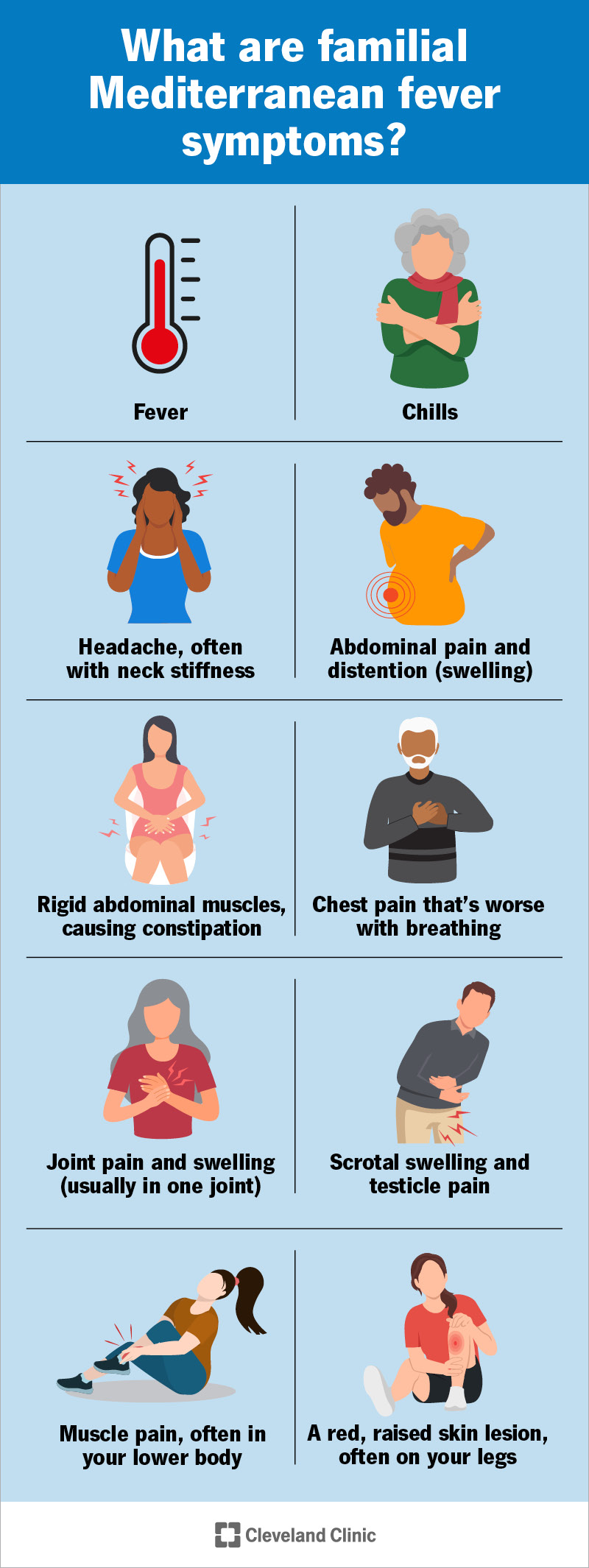
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/familial-mediterranean-fever-infographic)
Familial Mediterranean fever (FMF) is a genetic condition that causes episodes of fever and inflammation that come and go throughout your life. It’s named for the fact that it usually affects people from Mediterranean ethnicities.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
FMF is a recurrent fever syndrome. It causes inflammation in two types of membranes:
FMF episodes usually last a few days. During an episode, you’ll notice pain and other symptoms in your:
Familial Mediterranean fever symptoms usually first appear before you turn 20. They’re often severe in the early years. The episodes may happen less often and be less severe as you age. Between episodes, you may be symptom-free for weeks, months or years.
Visit a healthcare provider if you’re having pain, fevers or other symptoms that keep coming back. Early diagnosis and treatment can help you feel better and prevent potential long-term complications.
FMF symptoms can include:
Advertisement
The symptoms usually develop over several hours and last a few days. You probably won’t experience every symptom on this list. Fever is the most common. It’s often the only symptom in children.
You might notice warning signs of an FNF episode. They usually happen a few days before an episode starts. These are called prodromal symptoms. They include:
Episodes may occur randomly. But some people find they happen after specific triggers, including:
Genetic variations cause FMF. Specifically, changes in the MEFV gene. This gene helps create an important protein called pyrin. Your immune system relies on pyrin to work properly. When a changed MEFV gene makes the wrong kind of pyrin, your immune system doesn’t work like it should. This causes the inflammation and episodes of symptoms.
There are at least 30 genetic variations that can cause FMF. They’re most common in people from Mediterranean and Middle Eastern ethnicities. You may have a higher risk if your biological ancestry is:
Episodes of FMF are temporary. But they can take a toll on your body over time. Experiencing inflammation over and over again can overstress your immune system. This may lead to other health conditions. The most serious example is secondary amyloidosis.
Other complications of familial Mediterranean fever can include:
A healthcare provider will diagnose familial Mediterranean fever with a physical exam and some tests. They’ll discuss your health history and review any symptoms you’ve experienced. Tell your provider how often symptoms come and go, and when you first noticed them.
You might need blood tests to check for signs of inflammation during an episode. Your provider may suggest genetic testing to check for MEFV changes.
Your provider will monitor your body for changes after you start treatment.
Colchicine is the most common familial Mediterranean fever treatment. It’s an anti-inflammatory medication. Colchicine can help prevent or reduce the frequency of FMF episodes. It can also lower your risk of complications. It works for more than 9 in 10 people with FMF. You’ll probably need to take it every day for the rest of your life.
Advertisement
Your healthcare provider will suggest other medicines if it’s not safe for you to take colchicine or it doesn’t work. You might need:
You should expect to manage FMF for the rest of your life. Medication can manage the symptoms and reduce how often you experience them. But there’s no cure.
Many people stop having episodes with medication. Others have fewer, milder ones. You’ll have to take your medicine all the time, even when you’re not having symptoms.
Familial Mediterranean fever might sound like something you get on a family vacation. Unlike an infection you pick up on a cruise, FMF will probably be with you for the rest of your life. The good news is that it’s treatable. Your healthcare provider will help you find the right medication. Eventually, you’ll have milder symptoms that affect you less often.
Talk to your provider if it feels like the symptoms change or your treatments aren’t working as well as they used to. You know your body better than anyone. Trust your gut, and let your provider know if something seems off. They’ll help you keep an eye on any changes in your body and adjust your treatments if you need it.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When you have an inflammatory or autoimmune condition, you need experts by your side. At Cleveland Clinic, we’ll create an individualized treatment plan for you.
