Premenstrual syndrome, or PMS, is a combination of symptoms that arrive before your period. Your symptoms may be physical (like bloating or sore breasts), emotional (like irritability or sadness) or a combination of both. Either way, PMS symptoms can disrupt your life. Lifestyle modifications and over-the-counter medications can often relieve PMS symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
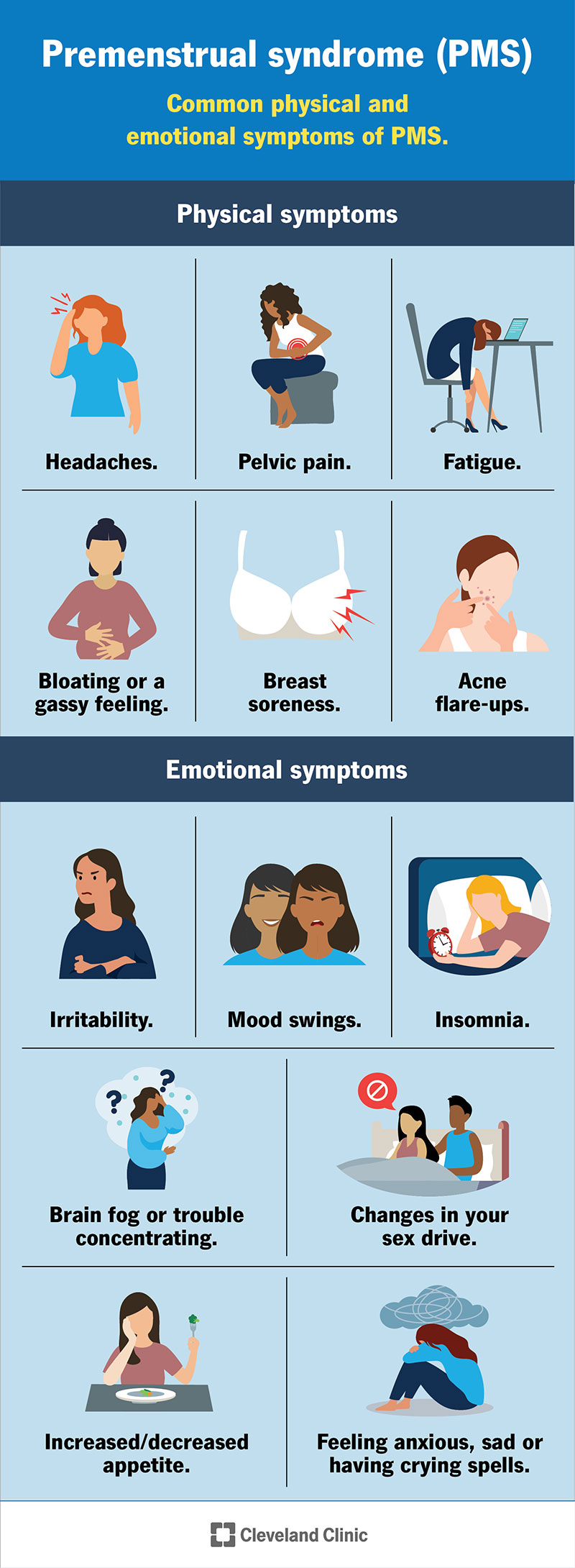
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24288-pms-premenstrual-syndrome)
Premenstrual syndrome, or PMS, describes physical and emotional symptoms that begin a week or two before your period. Most people who menstruate have at least one or more symptoms of PMS. These symptoms usually tip you off that your period is coming soon. Once you get your period, symptoms of PMS usually go away. These symptoms will often reoccur around the same time each menstrual cycle.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Almost 50% of people who menstruate say they have at least one PMS symptom. About 20% of those people have symptoms that are severe enough to disrupt their life.
PMS symptoms can be physical, emotional or a mix of both. They can also be mild, severe or somewhere in between. Not everyone experiences PMS. If you do, your symptoms may change throughout your life.
The most common physical signs of PMS are:
The most common emotional signs of PMS are:
The exact cause is unknown. But most healthcare providers believe PMS happens due to hormonal changes related to your menstrual cycle.
Symptoms usually show up around ovulation, when levels of estrogen and progesterone increase. Once your period begins, these hormone levels drop for a few days, and then, will start to rise again. These hormonal changes may be to blame for PMS. Some people are more sensitive to hormonal fluctuations, which may explain why PMS affects everyone differently.
Advertisement
Most people experience PMS symptoms about one to two weeks before their period. But the timing isn’t always exact. You can have PMS two weeks before your period or two days before your period.
You may be more likely to have PMS if you have:
Healthcare providers most often diagnose PMS in people who are in their late 20s and early 30s.
Your healthcare provider diagnoses PMS based on your symptoms. They‘ll ask you about what symptoms you have, when you have them and how they impact your life. To receive a PMS diagnosis, your symptoms must:
Questions your provider may ask include:
Your provider may also ask about your medical history and medications you’re taking to rule out factors other than PMS that may be causing your symptoms. They may ask you about your biological family’s medical history, too, as many conditions run in families. Your provider will rule out causes like:
There are many treatment options for PMS. Some people may need to try several different treatments until they find one that relieves their symptoms.
You can usually manage mild symptoms with over-the-counter (OTC) medications. More severe symptoms may require a prescription from a provider. Options include:
Advertisement
You can modify your lifestyle to help relieve pain and combat the mood-related symptoms of PMS. Examples include:
Vitamins, minerals and herbal supplements aren’t regulated by the U.S. Food and Drug Administration (FDA) the way over-the-counter and prescription drugs are, so it’s a good idea to check with a healthcare provider before taking them. Still, there’s some evidence that they can help with PMS:
Advertisement
PMS doesn’t go away for good until you experience menopause and no longer have periods. Until then, there’s plenty you can do to help manage your symptoms so they don’t disrupt your life. Keep tabs on when you tend to notice symptoms and take note of the treatments that relieve them. Put them to use each month when your symptoms usually begin.
PMS is common enough that many people accept it as an annoyance during “that time of the month.” Just because PMS is normal, it doesn’t mean you have to let it disrupt your life. Often, you can manage your symptoms with medications and lifestyle changes. If nothing you’re doing is making a big enough difference, see your provider to get treatments that can help.
Advertisement
You can’t prevent premenstrual syndrome, but you can manage symptoms with lifestyle changes, medications or a combination of both.
Contact a healthcare provider if you’re unable to get relief from your PMS symptoms. To get the most out of your visit, come to your appointment prepared to discuss your symptoms and your period in detail.
Be prepared to share:
You can use a pen and paper, a calendar or an app on your phone to track this information. This helps you and your provider recommend the best path forward.
If you have PMS, you may want to ask your provider:
Premenstrual dysphoric disorder (PMDD) is a severe and potentially debilitating form of PMS. It’s much less common than PMS, affecting about 3% of people who menstruate. With PMDD, you experience PMS symptoms but with much more intensity, especially when it comes to emotional responses and your mood. You’re more likely to experience anger, severe depression and anxiety with PMDD than with PMS.
There isn’t any solid evidence that PMS worsens at a particular age. Researchers believe PMS symptoms appear at similar rates across all age groups. Some people believe that their PMS symptoms tend to be more severe as they enter their 40s. But this is usually due to symptoms associated with perimenopause (like hot flashes or vaginal dryness).
Just because premenstrual syndrome (PMS) is common, it doesn’t mean that you have to tolerate the unpleasant symptoms it can cause. Pay attention to any aches and pains or mood changes that happen just before your period that may be signs of PMS. If they’re interfering with your well-being, try switching up your habits and taking over-the-counter medications that can ease your symptoms. If that doesn’t work, see a healthcare provider to get the treatment you need.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From routine pelvic exams to high-risk pregnancies, Cleveland Clinic’s Ob/Gyns are here for you at any point in life.
