Azotemia is a condition in which you have too much nitrogen, creatinine and other waste products in your blood. There are three different types of azotemia. Many people don’t notice symptoms, but some may include chest pain, swelling in your lower extremities, not peeing much and feeling tired. Treatment varies according to what type you have.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
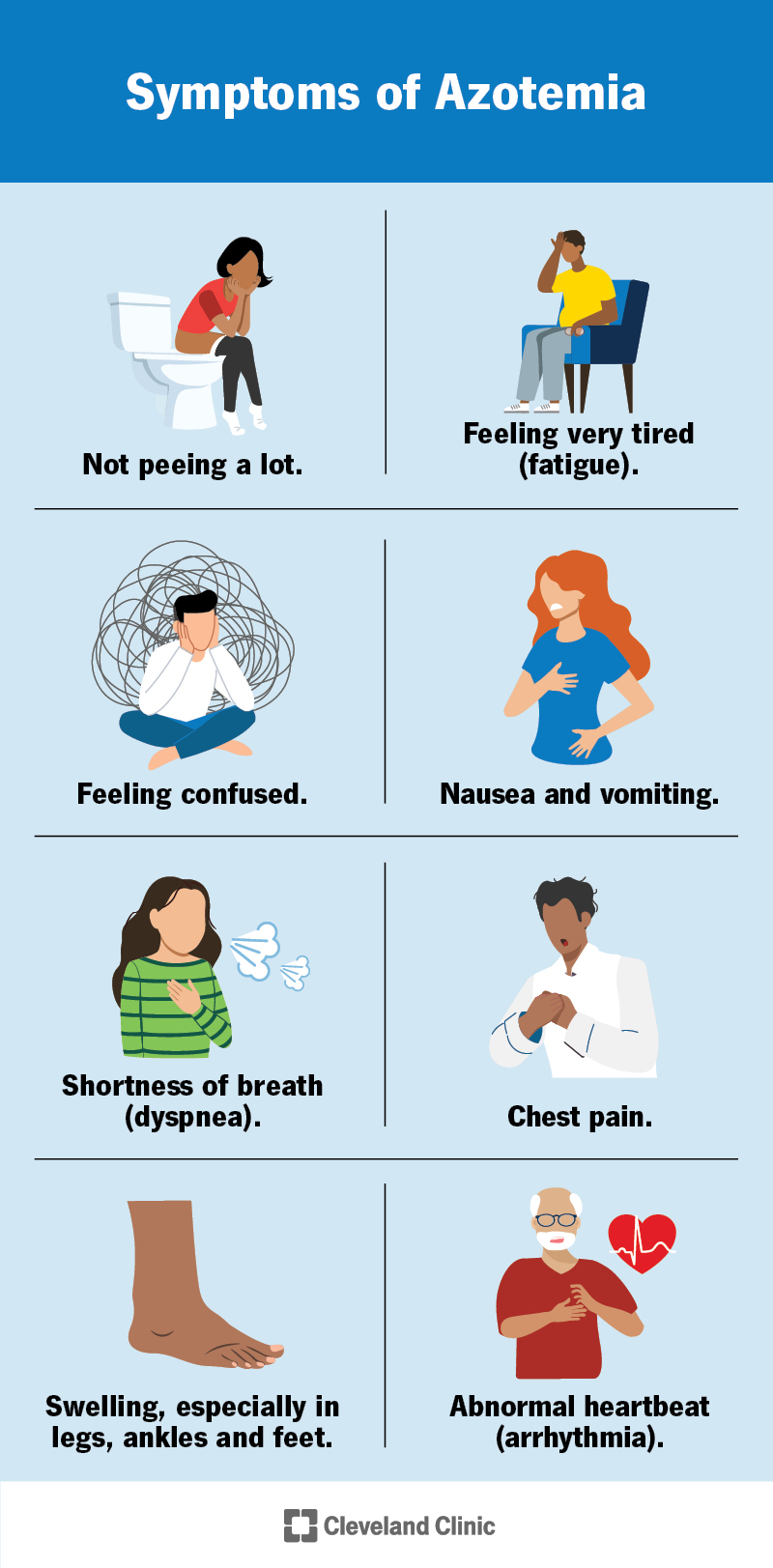
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/25037-azotemia)
Azotemia is a condition that happens when waste product levels in your blood are too high. Specifically, azotemia is when there’s too much nitrogen and waste products in your blood. These waste products develop when your body breaks down protein in foods and drinks you ingest. They form in your liver and travel in your blood to your kidneys. Healthy kidneys filter the waste products from your blood and leave your body through your urine (pee).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The three types of azotemia include:
No, azotemia isn’t the same as kidney failure (renal failure). Kidney failure is the main cause of azotemia.
Azotemia is common. It accounts for about 16% of hospital admissions.
Azotemia usually doesn’t have any symptoms that you can notice or feel until it reaches a later stage. Some people who have azotemia may not have any signs at any stage — a healthcare provider may discover you have it during tests for other conditions.
Advertisement
Azotemia symptoms may include:
Severe azotemia symptoms may include seizures or coma.
Azotemia causes depend on the type you have:
No, azotemia isn’t the same as dehydration. Dehydration is a common cause of prerenal azotemia. Dehydration may occur from:
No, azotemia isn’t contagious. You can’t spread azotemia to another person.
Anyone can get azotemia. However, you’re more likely to get it if you’re 65 or older.
Azotemia can lead to a dangerous buildup of waste products in your blood (uremia). Uremia often results from chronic kidney disease (CKD). Without treatment, uremia can be fatal.
Azotemia and uremia are both conditions that affect your kidneys.
Azotemia is when you have too much nitrogen and other waste products in your blood.
Uremia is when you have too much urea and other waste products in your blood. Urea is a type of nitrogen waste product that forms in your liver after proteins break down.
A healthcare provider who specializes in diagnosing and treating kidney conditions (nephrologist) will review your medical history, ask about your symptoms and conduct a physical examination. If they suspect azotemia, they’ll order a blood urea nitrogen (BUN) test and check your creatinine levels. Creatinine is a waste product of muscle tissue metabolism.
Advertisement
Tell your provider if you have a bleeding disorder or are taking any medications before your BUN test. They’ll disinfect your arm, use a thin needle to draw blood from a vein and then send your blood sample to a lab for testing.
An expected blood urea nitrogen range varies according to your age and sex. Levels higher than this range may indicate azotemia.
| Age and Sex | Normal BUN Level (mg/dL) |
|---|---|
| Children between 1 and 17 | Between 7 and 20 |
| Adult males | Between 8 and 24 |
| Adult females | Between 6 and 21 |
| Age and Sex | |
| Children between 1 and 17 | |
| Normal BUN Level (mg/dL) | |
| Between 7 and 20 | |
| Adult males | |
| Normal BUN Level (mg/dL) | |
| Between 8 and 24 | |
| Adult females | |
| Normal BUN Level (mg/dL) | |
| Between 6 and 21 |
A healthcare provider will also check your serum creatinine levels to diagnose azotemia. A serum creatinine range also varies according to age and sex. Levels higher than this range may indicate a kidney problem.
| Age and Sex | Normal Serum Creatinine Level (mg/dL) |
|---|---|
| Children between 1 and 16 | 0.2 to 0.9 |
| Adult males | 0.6 to 1.2 |
| Adult females | 0.5 to 1.1 |
| Age and Sex | |
| Children between 1 and 16 | |
| Normal Serum Creatinine Level (mg/dL) | |
| 0.2 to 0.9 | |
| Adult males | |
| Normal Serum Creatinine Level (mg/dL) | |
| 0.6 to 1.2 | |
| Adult females | |
| Normal Serum Creatinine Level (mg/dL) | |
| 0.5 to 1.1 |
Healthcare providers don’t use BUN to determine kidney failure. However, you likely have kidney failure if your BUN and creatinine numbers are higher than your baseline.
A healthcare provider may also order:
Advertisement
Azotemia treatment depends on which type you have, what’s causing it and its severity. A healthcare provider will conduct tests to determine its cause. Treatment options may include:
With early diagnosis and treatment, the outlook for many people who have azotemia is good.
However, without treatment, azotemia increases your chances of developing other severe medical conditions, including chronic kidney disease. It can also cause death. Follow your healthcare provider’s treatment plan to reduce your chances of developing these or other conditions.
The following tips can help you take care of your kidneys and prevent azotemia:
Advertisement
A healthcare provider will work with you to develop a treatment plan, which may include medications, changes to your lifestyle or a procedure. This may also include using medications sparingly, preventing dehydration and regular exercise.
If a healthcare provider diagnoses you with azotemia, schedule regular follow-up appointments. You should also schedule a visit if you notice changes in your symptoms or new pain.
Go to the emergency room if you notice symptoms of acute kidney failure. Symptoms may include:
Azotemia is a common condition that occurs when you have too many waste products in your blood. It develops after an injury or disease damages your kidneys and they’re not able to work as they should.
You may not realize you have azotemia because it often doesn’t cause any symptoms. It can be shocking to learn you have it. But healthcare workers will order tests to determine its cause and provide the best possible treatment. Talk to your providers about any questions or concerns you may have. They can answer your questions and provide support and advice on how you can best treat azotemia and take care of your kidneys.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a condition that’s affecting your kidneys, you want experts by your side. At Cleveland Clinic, we’ll work with you to craft a personalized treatment plan.
