Hypercapnia (hypercarbia) is when you have high levels of carbon dioxide in your blood. Carbon dioxide is a waste product that your body gets rid of when you exhale. If you can’t get rid of it, it can build up in your blood. COPD and conditions that affect your lungs, brain, nerves and muscles are the most common causes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
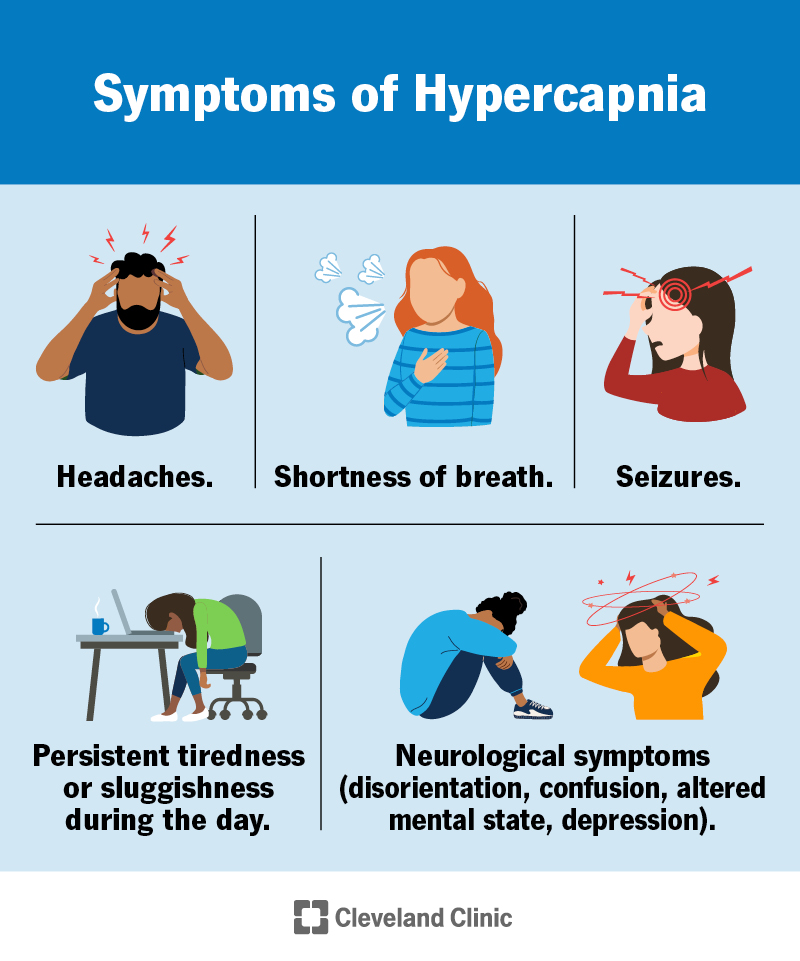
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24808-hypercapnia-hypercarbia)
Hypercapnia, also called hypercarbia, is when you have too much carbon dioxide (CO2) in your blood. Your body creates CO2 when your cells make energy. Your red blood cells carry it from your organs and tissues to your lungs, where you breathe it out. If your body can’t get rid of carbon dioxide, a waste product, it can build up in your blood.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hypercapnia can be chronic (long-lasting) and cause symptoms like shortness of breath (dyspnea) and daytime tiredness or fatigue. It can also be acute (sudden or all at once), with much more serious symptoms.
IMPORTANT: Acute hypercapnia is a medical emergency and can cause neurological (brain) symptoms like confusion, disorientation and paranoia.
Hypercapnia is when you have too much carbon dioxide in your blood. Hypoxemia is when you have too little oxygen in your blood. One can lead to another and you can be hypercapnic and hypoxemic at the same time.
Symptoms of hypercapnia include:
Chronic hypercapnia may cause vague symptoms like tiredness, headaches and shortness of breath. These may eventually lead to neurological symptoms like confusion. Acute hypercapnia can cause sudden neurological symptoms, headache and shortness of breath.
Any condition that increases CO2 levels or prevents CO2 from getting to your lungs and out of your body can cause hypercapnia. These include conditions that create hypoventilation or V/Q mismatch.
Advertisement
Hypoventilation happens when you breathe too slowly or shallowly to remove carbon dioxide from your body. V/Q mismatch is when your body has enough air coming into your body (ventilation, or “V”) but not enough blood flow to your lungs (perfusion, or “Q”), or vice-versa. This can happen if you have a lung disease that creates “dead space,” or areas that aren’t getting blood flow, in the small air sacs in your lungs (alveoli). Your lungs fill with air but can’t remove all of the CO2 from your blood.
Chronic obstructive pulmonary disease (COPD) and sleep apnea are two common conditions that sometimes lead to hypercapnia. Others include:
Fever and exercise can increase your CO2 levels, but most people’s bodies make adjustments to bring their bodies back into balance. Sometimes, giving oxygen to someone with COPD can cause hypercapnia.
Heart, lung, muscle and neurological (brain and spinal cord) conditions put you at higher risk for hypercapnia. Using medications that sedate you (like opioids or benzodiazepines) can cause you to breathe more shallowly or less frequently, increasing your risk of hypercapnia.
If your body can’t compensate for high carbon dioxide levels, it can lead to life-threatening conditions. These include:
To diagnose hypercapnia, providers use special blood tests to measure the carbon dioxide in your blood. They may use other tests to determine possible causes of hypercapnia.
Tests to diagnose hypercapnia or its underlying causes include:
Advertisement
Treatment for hypercapnia depends on the cause. Providers may treat you with:
Giving oxygen to someone with COPD can sometimes make hypercapnia worse. This is because it can increase V/Q mismatch or cause your red blood cells to release CO2 into your blood (Haldane effect) that your body can’t effectively get rid of.
The outlook for hypercapnia depends on the cause. Many causes are reversible if caught early. Chronic hypercapnia caused by sleep apnea can be prevented with a device your provider prescribes or certain types of surgery.
Some studies suggest that people with COPD who have hypercapnia have a worse prognosis than people with COPD who don’t have hypercapnia.
The best way to prevent hypercapnia is to take all medications as prescribed and manage any underlying conditions. If you have COPD, talk to your provider about how to manage exacerbations (flare-ups).
Advertisement
Managing any underlying conditions that put you at risk for hypercapnia is the best way to take care of yourself. If you have COPD, sleep apnea or any other condition that puts you at risk for hypercapnia, talk to your provider about symptoms to look out for.
Talk to your healthcare provider if you have symptoms of hypercapnia, especially if you have another condition that puts you at risk.
Go to the nearest emergency room or seek care immediately if you have any signs of serious illness, including:
It might be helpful to ask your provider:
Our bodies balance themselves all the time, without us even thinking about it. Oxygen and carbon dioxide levels can go up or down and our bodies adjust. But certain conditions can make it harder for our bodies to balance as they need to. This can lead to conditions like hypercapnia.
The excess carbon dioxide in hypercapnia can cause life-threatening complications. If you have a condition that puts you at risk for hypercapnia, make a plan with your provider about what to do if you have any worrisome symptoms. See a provider right away if you have symptoms of hypercapnia. Go to the ER if you have any mental changes like confusion, seizures or disorientation.
Advertisement
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Need care fast? Cleveland Clinic’s Express Care and Urgent Care locations treat everything from sprains to sinus infections — no appointment needed.
