Heart inflammation happens after you have an injury or infection in your heart. This rare condition can be mild, serious or in between the two extremes. Mild cases don’t need treatment, and medication helps with all three types of carditis. Recovery can take many weeks. If you have a bad case, you may need procedures or a medical device.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
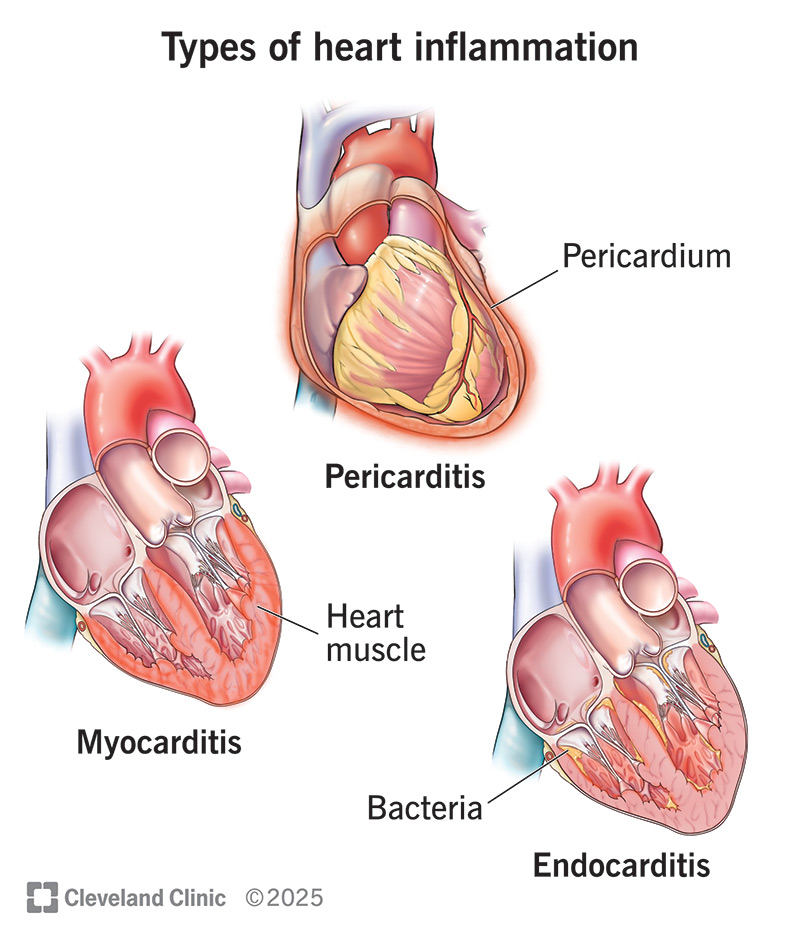
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23052-heart-inflammation)
Carditis (heart inflammation) is a condition that happens when your heart is hurt or infected. This can happen to your heart’s muscle, the sac around your heart or the lining of your heart’s chambers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
For some people, inflammation of the heart happens without warning. For others, it takes longer. Some people have severe symptoms, while others barely have any symptoms. The degree of inflammation can also vary from person to person, depending on individual factors and causes.
Carditis affects three different areas of your heart. All three types of heart inflammation are rare:
Common symptoms for all three types of heart inflammation include chest pain, shortness of breath and fever.
Other signs of carditis are more specific to the type you have, like:
Advertisement
When a virus causes heart inflammation, you can have symptoms from the virus first.
Infections — usually from viruses or bacteria — cause most cases of heart inflammation. These can range from HIV or COVID-19 to herpes and others. Lyme disease bacteria can lead to Lyme carditis. Rheumatic fever can cause rheumatic carditis.
Other causes of an inflamed heart include:
People in any age group can get heart inflammation, but it’s more common in males. Certain medical issues or treatments put you at a higher risk of an inflamed heart. These include:
You can’t change your age or the medical conditions you have that put you at risk for heart inflammation. But there are a few things you can control, including:
If you’re at high risk for endocarditis, your healthcare provider can prescribe antibiotics. You take these before going to the dentist or having surgery. You’re at high risk if you’ve had endocarditis before, had a valve replaced or have had a specific heart issue since birth.
You can get carditis more than once, so be on the lookout for symptoms.
A mild case of pericarditis or myocarditis can go away on its own. But some complications of heart inflammation are serious and can be life-limiting. Without treatment, heart inflammation can cause:
To detect carditis, your healthcare provider will perform a physical exam and collect your medical history. They’ll do blood tests and other tests to help them rule out a heart attack and find the infection’s source. Your provider will also check for fluid around your heart. They’ll look at how well your heart is functioning and see if it’s working normally.
Tests include:
Advertisement
Treatment for carditis varies. Medications can help you fight infections and keep your immune system and heart from working too hard. If you have more serious complications, you may need procedures or medical devices.
Medicines for heart inflammation may vary depending on which part of your heart is inflamed. Medications you take may include:
For some cases of carditis, you may need a procedure or surgery to:
Contact your healthcare provider if you get any new symptoms while you’re recovering. Since chest pain is a common symptom of carditis and a heart attack, you may not know which one is happening. To be safe, call 911 (or your local emergency service number) if you’re having chest pain.
When you visit your provider, you may want to ask:
Advertisement
It can take several weeks or years to recover from some types of heart inflammation. Once you see your healthcare provider, be sure to follow their instructions for taking medicines they prescribed. You’ll also need follow-up appointments throughout your recovery. These may include repeat blood tests or imaging.
Follow-up visits are important because carditis can come back months or years later.
Carditis can be mild, life-threatening or somewhere in between. The prognosis (outlook) is generally good when you get treatment quickly. You might not even need treatment for a mild case. After treatment, you might not have issues, or you might still need medicine. You may need a heart transplant at some point.
Feeling a pain in your chest or having a hard time breathing makes you stop what you’re doing. If you think you have carditis, don’t wait to get help. You’ll have the best outcome if you catch heart inflammation early.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart needs some help, the cardiology experts at Cleveland Clinic are here for you. We diagnose and treat the full spectrum of cardiovascular diseases.
