A corneal ulcer is an open sore on your cornea. It’s considered a medical emergency. Infections are the leading cause. Symptoms include a red or bloodshot eye, watering eye, severe eye pain, and pus or other eye discharge. In severe cases or cases with delays in treatment, a corneal ulcer is more likely to cause vision loss and blindness.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
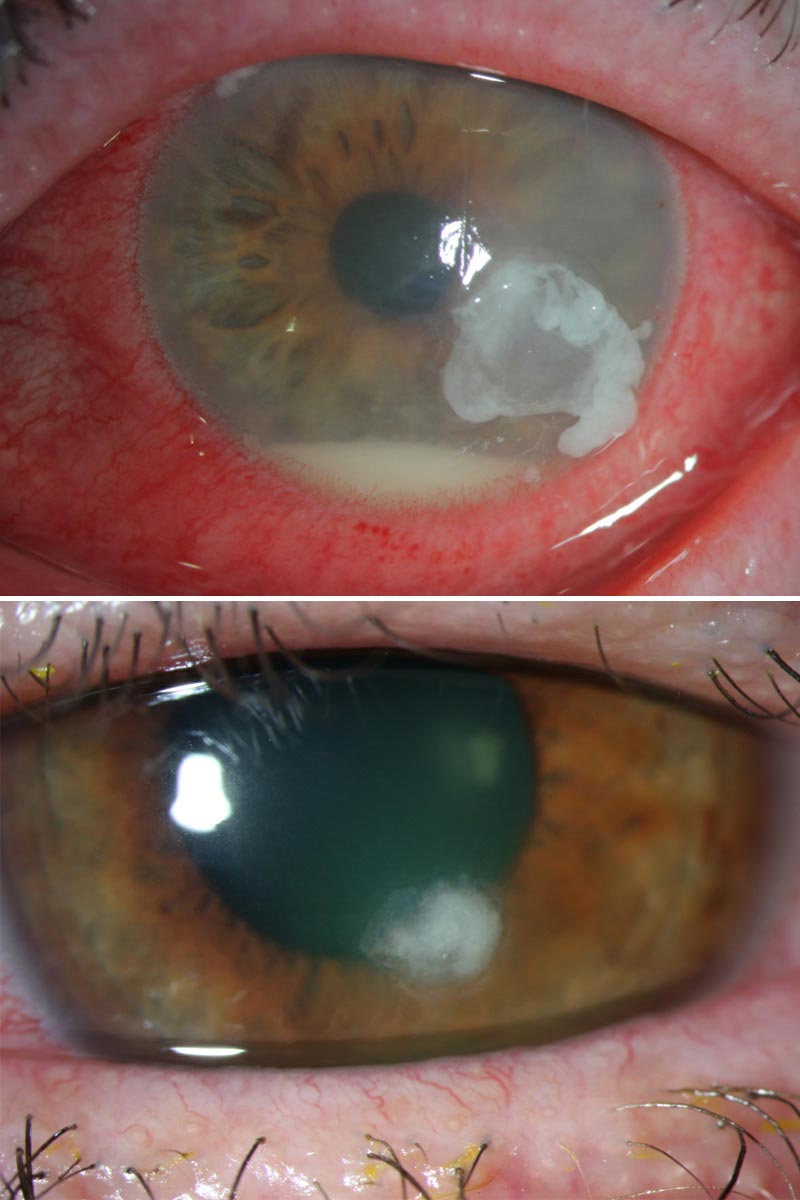
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/22524-corneal-ulcer)
A corneal ulcer is a wound-like sore on your cornea, the clear, dome-shaped tissue layer at the front of your eye. Corneal ulcers can happen for several reasons, but they usually happen because of infections.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your corneas are like a windshield on a car. They protect the inside of your eyes from the outside world. Damage to your cornea can create imperfections that are more vulnerable to infections and other issues. Having a corneal ulcer is like having a crack or chip in that windshield. Corneal ulcers are a medical emergency. They need immediate care because they can cause permanent eye damage, low vision and even blindness (especially without treatment).
Corneal ulcer symptoms vary widely. The most common ones include:
Corneal ulcers can happen for many reasons, but they mainly break down into two categories: infectious and noninfectious.
Infectious causes are conditions that you can catch from or spread to others. There are four subtypes of infectious causes:
Advertisement
These are conditions or circumstances that can cause corneal ulcers without an infection. Examples include:
Anyone can get corneal ulcers, but you have a higher risk if you have:
Advertisement
Corneal ulcers can cause the following complications:
To diagnose a corneal ulcer, an eye specialist or another healthcare provider will rely mainly on an eye exam. Unlike a routine exam that checks all parts of your eye health, these exams will be more issue-specific. A key part of the eye exam that they’ll use is the slit lamp exam. It lets your eye specialist get an up-close, detailed look at your corneas.
One particular lab test your provider might do is a swab culture. That involves taking a soft-tipped swab, collecting some of the discharge from your eye and then sending that to a lab for testing. The test results may tell your provider what kind of infection is causing your ulcer. In cases that aren’t responsive to treatment, your provider may recommend taking this a step further and doing a corneal biopsy. That involves taking a sample of your corneal tissue for testing.
Your eye specialist can tell you more about any other tests they recommend. They can also explain how the tests work, why they should help and any side effects you should expect after the tests.
Advertisement
Corneal ulcers can happen for many reasons, which means there are many ways to treat them. Some treatments are very specific and only work for certain conditions. Other treatments are more general, helping the symptoms that are most likely with corneal ulcers.
Some of the more common treatment options include:
Advertisement
Other treatments may be possible or necessary, depending on your specific circumstances. Your eye specialist is the best source of information about the treatment options available for your specific case. They can also tell you more about the possible side effects or complications from treatment.
Corneal ulcers can vary widely depending on what causes them. That includes how long they take to heal or how well they should heal. Your eye specialist can tell you more about what you can expect with your specific case.
Some key factors that can impact your outlook are:
The healing time for corneal ulcers can vary widely, and many factors play a role in this. Your eye specialist is the best person to tell you the likely timeframe for your case, as they can tailor the estimate to the details of your situation.
Corneal ulcers aren’t 100% preventable, but there are many things you can do to lower your odds of developing them. Some things you can do include:
If you have a corneal ulcer, the most important things you can do include:
Your eye specialist can tell you what symptoms mean you need to call them or seek medical care. That generally includes symptoms like:
You may want to ask your eye specialist the following:
Wearing contacts for long period blocks oxygen from reaching your eyes. Also, bacteria on the lens — transferred from your finger when inserting or from non-sterile cleaning solutions — can get trapped under your lens. These factors raise the risk of infection, which can lead to a corneal ulcer.
A contact lens wearer is about 10 times more likely to get a corneal ulcer than someone who doesn’t wear contacts. Someone who sleeps in contact lenses is about 100 times more likely to get an ulcer than someone who doesn’t wear contacts.
A corneal abrasion is a scrape or scratch on your cornea. These corneal injuries usually heal on their own
A corneal ulcer is an open sore on your cornea. Infections, dry eye and other conditions cause a corneal ulcer.
These eye conditions are closely related.
A corneal ulcer is an open wound — a loss of corneal tissue — that’s often the result of an eye infection.
Keratitis is a more general term for a group of disease processes that cause inflammation of your cornea. Eye infection, injury and wearing contact lenses too long — some of the same causes of corneal ulcer — also cause eye inflammation. Keratitis can lead to a corneal ulcer.
Both conditions can lead to vision loss.
Corneal ulcers are a vision-threatening eye emergency. Even a minor eye injury can lead to a corneal ulcer. If you think you have symptoms of a corneal ulcer, contact your eye care provider right away. They will examine your eye, make the diagnosis and start treatment. If you wear contact lenses, make sure you know how to properly insert, clean and store them. Your eye care team can teach you proper techniques and answer all your other questions.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Getting an annual eye exam at Cleveland Clinic can help you catch vision problems early and keep your eyes healthy for years to come.
