Recurrent corneal erosion is a condition that happens when outer layers of your cornea separate. Usually this happens due to past injuries that disrupted the bonds between those layers. These erosions are painful and disruptive, but there are many ways to treat them. They usually respond to treatment, but some people will have recurrences.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
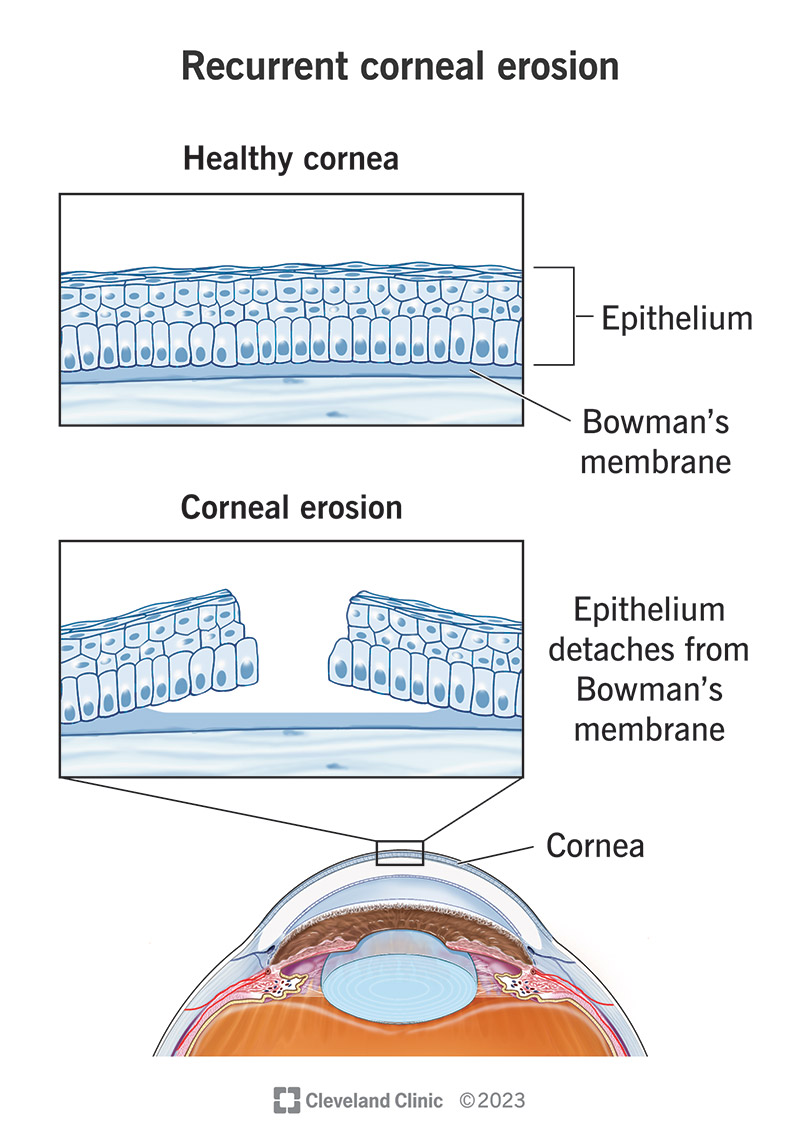
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/recurrent-corneal-erosion)
Recurrent corneal erosion (RCE) happens when the outer layer of the cornea, the transparent membrane at the front of your eye, separates and lifts away from underlying layers. It’s a painful condition that causes your eyes to tear and water, and it makes bright light painful. RCE can cause short-term vision issues and long-term eye damage when not treated.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The cornea is like the windshield of your eye. It’s there to keep the inside of your eye safe and separate from the outside world. The cornea has five layers. Recurrent corneal erosions affect the outermost two. Those layers are:
When you have RCE, the epithelium and Bowman’s membrane don’t stick together as they should. That can cause the epithelium to erode, exposing vulnerable layers underneath. And corneal erosions are very painful because the epithelium is packed with nerve endings.
RCEs are common, but experts aren’t sure exactly how often they happen. One study in London, England found they affect just under 1% of that city’s population in a year. But that probably underestimates the true number because people may not seek medical care for minor erosions. That’s because your cornea repairs itself very quickly, so minor erosions may be gone within minutes or hours.
Advertisement
If you have RCE, it’s common to experience symptoms when you first wake up. Opening your eyes can lift away the outer cornea layer if the bonds that join it to the underlying layer aren’t strong enough. That can lead to any of the following eye symptoms:
RCE is similar to what happens if you apply a fresh coat of paint over a layer of damaged, peeling paint. The damaged underlying paint keeps the new paint from sticking correctly. Even lightly passing your hand across the newly painted surface can cause the new layer to lift and peel off.
The most common cause of RCE is an earlier eye injury. Those injuries are usually from things like your fingernails, paper or contact with some part of a plant (like a tree or shrub). They also don’t have to be recent. Some people will have an RCE related to an eye injury that happened years earlier. The symptoms of injury-related RCEs usually affect only one eye.
Corneal diseases and chronic conditions that affect your eyes are also common causes or contributing factors to RCEs. These often affect just one eye, but some people will have symptoms in both eyes.
These conditions include:
RCE complications are usually not life-threatening, but they’re still disruptive and serious. They include:
RCEs are generally easy to diagnose. A healthcare provider, such as an optometrist or ophthalmologist, can diagnose it by asking questions about your symptoms, medical history and any previous issues or injuries affecting your eye.
Providers can then confirm the diagnosis using certain tests. That stops the pain from RCE and prevents discomfort during tests. The possible tests include:
Advertisement
Providers use a stepped approach to treat RCE. They’ll generally start with simpler medical treatments and move to more advanced surgical treatments if simpler ones don’t help. They may also skip to more advanced treatments if you have a more severe RCE.
Medical management aims to make it as easy as possible for your eye to heal on its own. Many of the treatments are ones you can give to yourself. Your provider will give you specific instructions on what you’ll need to do.
Some of these treatments will need to continue for days or weeks. You may need to do others for months, depending on the severity of your RCE.
Medical management can involve one or more of the following treatments:
Advertisement
Advertisement
Surgical treatments involve removing damaged sections of epithelium so it can regrow uniformly instead of in uneven patches. These procedures usually happen under topical anesthesia, which numbs the surface of your eye to prevent pain or discomfort.
After these treatments, your healthcare provider may also treat you with medicines like those listed above. The epithelium usually regrows within a few days, but medical treatments may need to continue for weeks or months to ensure the epithelium bonds securely to underlying layers.
Surgical treatments can involve one or more of the following:
The complications or side effects of the treatments vary depending on many factors, especially the specific treatment(s) you receive. Your healthcare provider is the best person to tell you about the side effects or complications you’re most likely to experience and what you can do to limit or prevent them.
The recovery time after treatment varies depending on several factors. The epithelium layer of your cornea can regrow and repair itself very quickly. But it can take weeks or months for the underlying layers to repair and bond to each other fully. Your provider can tell you about the likely recovery time, and when you should notice changes in symptoms, vision or how your eye feels.
If you have RCE, the main symptom is pain. Other symptoms are common, unpleasant and disruptive, but minor erosions usually heal rapidly. It’s common for people only to seek medical care when erosions are moderate to severe.
The main issue you may deal with is that they can happen repeatedly. And the more they happen, the more likely it is to cause complications that affect your vision.
Because of that, the best thing to do is see an eye specialist if you notice RCE symptoms, especially when you wake up and open your eyes in the morning. Early treatment can limit damage from an RCE and reduce the risk of future ones.
Your cornea has tremendous regenerative ability. It can repair minor damage within hours and more severe damage within days.
But it’s also important to remember that RCEs occur when healing doesn’t happen correctly. When that’s the case, you may need to consistently apply medications or other treatments to your eyes as prescribed for weeks or even months. While that might seem tedious and troublesome, it’s also the best way to ensure that your eyes heal properly and you avoid future RCEs.
RCEs are painful, unpleasant and sometimes serious, but they aren’t life-threatening. Sometimes they recur, but recurrences are usually treatable. And fortunately, complications that might affect your vision long-term or permanently are rare.
RCEs can happen unpredictably. You can’t prevent them for certain, but you can do things to make them less likely to happen.
The most important way to prevent RCEs is to prevent eye injuries. Wear eye protection like goggles, masks or safety glasses whenever there’s a chance of injury to your eye. That’s particularly the case if you’re working with tools or around objects that could impact your eyes.
Lubricating the eyes with artificial tears, gel or ointment at bedtime can be especially useful, especially if you have eye pain when you wake up. The lubrication between the corneal surface and the eyelid can help prevent the sticking that contributes to erosions.
If you think you have an RCE, getting treatment early is the best plan of action. That way, you get treatment and relief for your symptoms and reduce the odds of future issues.
If you have an RCE, your provider will guide you on managing it. It’s important to follow their instructions exactly. The closer you follow the instructions and take medications or treatments as prescribed, the more likely you’ll recover without complications.
If you have an RCE, you should see your healthcare provider as recommended for follow-up visits. Doing so will let them track the healing of your cornea and adjust your treatments if necessary. You should also call or see them if you notice changes in your symptoms, your vision or the effectiveness of the treatment(s) you take.
RCE is usually not an emergency condition, but it can be painful and extremely disruptive. If you have RCE symptoms, calling your primary care provider’s office for guidance is a good idea. You may also choose to go to an urgent care-type clinic.
While RCE is usually not an emergency, it does have similarities to more severe eye injuries, like corneal lacerations. When in doubt, get emergency care. Doing so without delay may make a big difference in treatment, recovery and preserving your eyesight.
If you have eye pain along with the following, you should get medical attention:
When your eyes work as expected, it’s easy not to think about how much you use them. But it can be particularly scary when your eyes hurt and you don’t know why. RCEs are serious and painful, but they’re also very treatable.
If you have RCE symptoms, especially if they’re new, talk to a healthcare provider or eye specialist. Early diagnosis and treatment will give you the best odds of a fast recovery and preventing future occurrences.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s ophthalmologists and optometrists have the highest training available. We provide exams, vision correction and care for many eye conditions.
