Torsades de Pointes is a specific type of ventricular tachycardia, a fast heart rhythm that begins in your heart’s ventricles. Symptoms include heart palpitations, dizziness and fainting. Cardiac arrest is also possible. Some people don’t have symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
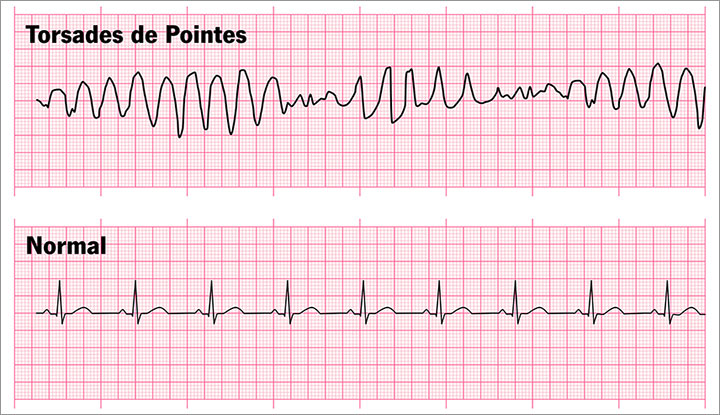
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21915-torsades-de-pointes-vs-normal)
Torsades de Pointes is a rare, dangerous type of fast heart rhythm (tachycardia) that starts in your heart’s ventricles (lower chambers). This condition can cause a heart rate from 150 to 300 beats per minute. A normal pulse rate is 60 to 100 beats per minute. Torsades de Pointes can lead to sudden cardiac death without any warning symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An electrocardiogram (EKG) will show a specific pattern of ventricular tachycardia that looks like twisting points or peaks (which is what the name means in French).
If you have a long QT interval and your ventricles get an extra beat during the time when they’re supposed to be getting ready for the next beat, you may get Torsades de Pointes. The QT interval is the time between when your ventricles beat (QRS) and when they fully relax before the next beat (T).
Half of the people with this condition don’t have any symptoms. People who get Torsades de Pointes symptoms can have:
Some people are born with long QT syndrome, an electrical problem with their hearts, which can lead to Torsades de Pointes. More commonly, certain medicines and low electrolytes lengthen your QT interval. This can put you at risk for Torsades de Pointes.
Medicines that can cause Torsades de Pointes include:
Some risk factors are harder to control than others. Risk factors for Torsades de Pointes include:
Advertisement
If long QT syndrome runs in your family, a healthcare provider can test you to see if you also have it. If you inherited long QT syndrome from a parent, talk to a heart rhythm specialist before you start an exercise program.
You can reduce your risk of Torsades de Pointes in these ways:
Possible complications of Torsades de Pointes include:
Your provider can see a long QT interval and a distinct pattern that looks like twisting points or peaks on an electrocardiogram (EKG).
Other tests to diagnose Torsades de Pointes include:
Torsades de Pointes treatment may include medications and procedures. If you inherited long QT syndrome from your parents, your treatment will include more long-term solutions than someone who got a long QT interval from a medication.
Your provider may stop giving you medicines that could cause Torsades de Pointes. Medicines they may start giving you may include:
Your provider may use one of the following treatments:
If you’re in the hospital for Torsades de Pointes, you’ll need a follow-up visit two weeks after you go home. Because of your risk of sudden death, you need regular follow-up visits with a cardiologist (heart expert).
Also, let your provider know if you’ve had bad side effects from medicines.
You should go to the emergency room if you have a very fast pulse rate, you feel palpitations, dizziness or lightheadedness, or you get fainting episodes.
Questions to ask your healthcare provider may include:
Advertisement
You’ll stay in the hospital until your heart rhythm is under control. A fast heart rhythm (ventricular tachycardia) from Torsades de Pointes often stops by itself. But without treatment, it will come back often. It can also lead to ventricular fibrillation.
If you don’t get treatment, Torsades de Pointes could become fatal. With treatment, your chances of survival are good, especially if you stop taking the medicine that caused the long QT interval.
Having an abnormal heart rhythm is unnerving. But your outlook with Torsades de Pointes is good if you follow your provider’s instructions and keep your follow-up appointments. Getting basic life support training for your family may give you peace of mind in case you need help.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
