Defibrillation can be a lifesaver for someone in cardiac arrest by using an electrical charge to stop your heart’s abnormal rhythm. This allows your heart to start a normal rhythm again. Defibrillation isn’t a guarantee of survival. Cardiac arrest is still fatal for many and survivors often need different types of therapy to recover.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
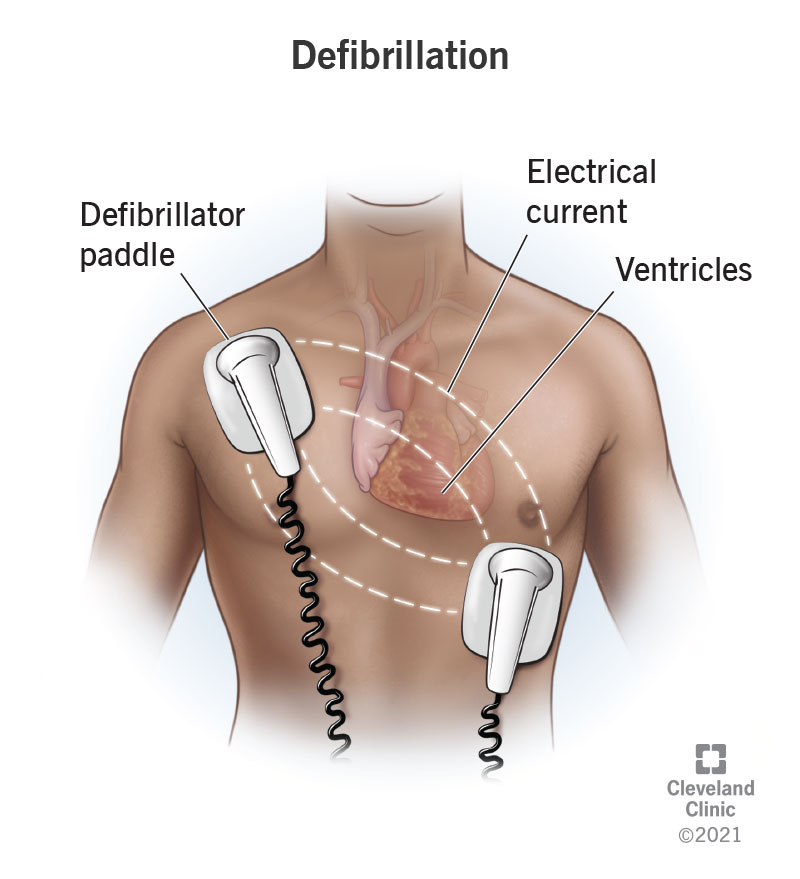
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/23021-defibrillation)
Defibrillation is the use of an electrical current to help your heart return to a normal rhythm when a potentially fatal arrhythmia (abnormal heart rhythm) is happening in your heart’s lower chambers (ventricles). Also known as electrical cardioversion, defibrillation is most effective when a healthcare provider delivers the shock as soon as possible after an arrhythmia starts.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Defibrillation can help with:
Someone with the specific types of arrhythmias named above may need defibrillation. If they’re in a hospital or a place that has an automated external defibrillator, someone can help them. But those who are at a high risk of a potentially fatal heart rhythm need to have a defibrillator on their person at all times.
Shocks from personal defibrillators can range from painless to pain that feels like someone kicked your chest.
People at risk for a dangerous arrhythmia may use:
Defibrillation gives you a chance to survive sudden cardiac arrest. You can give cardiopulmonary resuscitation (CPR) until someone can provide defibrillation. You can perform defibrillation even if the person has a pacemaker or an implantable cardioverter defibrillator (ICD).
Advertisement
Each year, more than 184,000 people outside of hospitals and about 200,000 people in hospitals experience cardiac arrest in the United States and may receive defibrillation.
Your first responder or healthcare provider will keep doing CPR until a defibrillator is ready and charged.
When they’re about to deliver the shock, they’ll make sure no one is touching the person receiving the shock (or their bed).
An automated external defibrillator (AED) — found in airports and other public places — can examine your heart’s rhythm to figure out if it’s the type of arrhythmia that needs a shock. It charges itself and then gives verbal instructions for using it.
Your healthcare provider will follow these steps for a cardiac defibrillation procedure:
Defibrillation briefly stops your moving heart muscle to allow your heart to generate an electrical impulse and start a normal rhythm. In essence, defibrillation restarts the heart.
Your provider will do CPR again for two minutes, check to see if you have a pulse and look to see if your heart rhythm is normal. If necessary, they’ll do more CPR and give you another shock. They’ll also give you medicines (epinephrine or amiodarone) if defibrillation didn’t work.
If you’re still unresponsive after your blood is moving again, you may need to have your body temperature cooled to 89.6 to 96.8 degrees Fahrenheit (32 to 36 degrees Celsius). Once you’re stable, you may need cardiac catheterization.
Defibrillation can save your life if you receive it within the first 10 minutes of having ventricular fibrillation.
If you perform defibrillation on someone who doesn’t have ventricular tachycardia (with no pulse) or ventricular fibrillation, you may cause ventricular fibrillation and cardiac arrest.
Recovering from cardiac arrest and defibrillation is a long-term effort of months or years for many survivors. After cardiac arrest, up to 40% of survivors have some level of impairment that keeps them from going back to work or doing regular daily activities when released from a hospital. Many survivors deal with fatigue. You also may need time to recover from a rib fracture from CPR and deal with other issues, like seizures or trouble walking. You may need occupational, physical and/or speech therapy.
Advertisement
If you see someone collapse, call 911.
People who survive ventricular fibrillation are very likely to have it happen again. This is why your healthcare provider will treat the cause of your ventricular fibrillation and/or give you an ICD. You’ll need regular checkups to be sure your ICD is doing its job. It also needs a battery replacement after five years or so.
If you’ve received defibrillation or have an ICD, keep taking medicines your healthcare provider prescribed for you. You’ll also need to visit your provider regularly to make sure your ICD is working right. If your defibrillation happened in an emergency situation, you may need months or years to get your body back to how it was. Getting physical therapy and other types of therapy can help you improve, but they take time and patience.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
When your heart rhythm is out of sync, the experts at Cleveland Clinic can find out why. We offer personalized care for all types of arrhythmias.
