Psoriatic arthritis is a form of arthritis that’s linked to psoriasis — a chronic skin condition. The most common symptoms are joint pain and stiffness, skin rashes and changes in your fingernails and toenails. There’s no cure for psoriatic arthritis, but a healthcare provider will help you find treatments to manage your symptoms.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Video playlist content: This video playlist is available to watch online.
View video playlist online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_qg0j86ei/flavorId/1_5f3sgelj/format/applehttp/protocol/https/a.mp4)
Learn more about psoriatic arthritis, it's symptoms and possible treatment options.
Psoriatic arthritis is a type of arthritis. It usually affects people who have psoriasis or a biological family history of psoriasis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Arthritis is a common disorder that affects your joints. It causes pain and inflammation in and around your joints. Psoriasis causes inflammation in your skin. Psoriasis rashes are patches of discolored skin covered with scales. These thick, scaly areas are called plaques. It can also make your fingernails and toenails thicken and look flaky or pitted (covered in tiny indentations).
Both arthritis and psoriasis are autoimmune diseases. An autoimmune disease is the result of your immune system accidentally attacking your body instead of protecting it. Psoriatic arthritis happens when you develop psoriasis symptoms on your skin and inflammation in your joints.
Psoriatic arthritis symptoms on your skin and in your joints usually come and go in periods called flares. A healthcare provider will suggest treatments to relieve your symptoms during a flare.
Visit a healthcare provider if you notice new symptoms on your skin or pain, swelling or stiffness in your joints.
Less than 1% of all people experience psoriatic arthritis. But it’s much more common in people who have psoriasis. Around 30% of people with psoriasis develop psoriatic arthritis at some point in their life.
A healthcare provider might classify psoriatic arthritis based on which joints it affects or on which side of your body you experience symptoms. The five forms of psoriatic arthritis include:
Advertisement
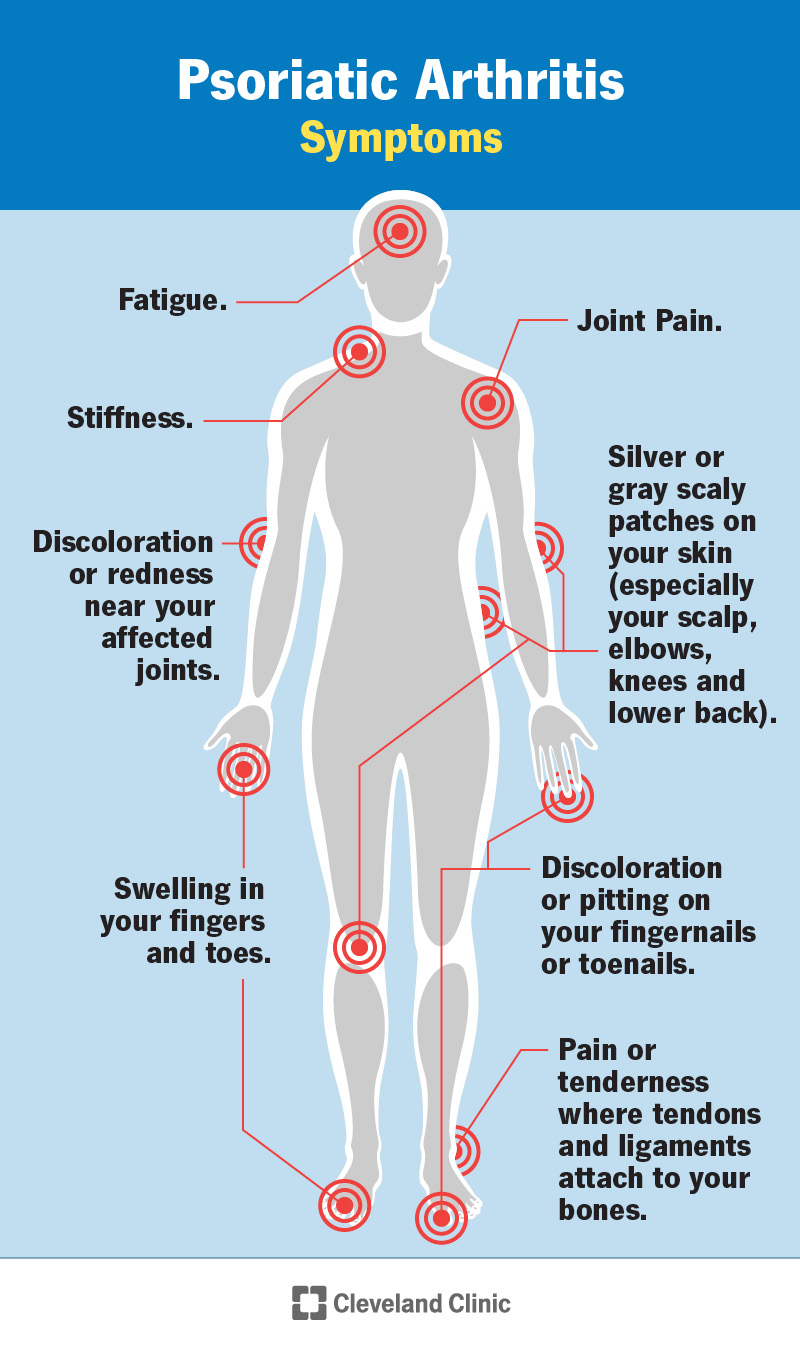
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/13286-psoriatic-arthritis-infographic)
Psoriatic arthritis can affect any joint in your body. Your symptoms can be mild — only a small amount of pain and stiffness with few signs of psoriasis on your skin. More severe psoriatic arthritis flares can make it hard or impossible to move and use your joints and will cause larger patches of psoriasis on your skin.
The most common psoriatic arthritis symptoms include:
Experts aren’t sure what causes psoriatic arthritis. Some studies have found that people with psoriatic arthritis have similar genetic mutations. Experts can’t say for certain if these changes in your genes are what cause psoriatic arthritis or if they change after you develop it.
Around 40% of people with psoriatic arthritis have a family member that also has it. This means it might be a hereditary condition — passed from biological parents to their children.
Advertisement
Tell your healthcare provider if someone in your family has psoriasis or psoriatic arthritis.
Psoriatic arthritis can affect anyone. It usually develops in people between 30 and 50.
People with psoriatic arthritis typically develop psoriasis in their teens or early 20s and don’t develop symptoms in their joints until later in life.
People with psoriatic arthritis are more likely to develop other health conditions, including:
Psoriatic arthritis symptoms can make it painful or difficult to use your joints. This can make it hard to get enough exercise. Talk to a healthcare provider about low-impact exercises that put less pressure on your joints. Yoga, walking or aqua therapy are all good ways to work out without stressing your joints.
A healthcare provider will diagnose psoriatic arthritis with a physical exam and some tests. Your provider will ask you about your symptoms and look at your skin and joints.
You might need to visit a rheumatologist, a provider who specializes in treating musculoskeletal conditions, autoimmune disorders and inflammatory conditions. A dermatologist — a provider who specializes in taking care of your skin — can diagnose and suggest treatments for psoriasis.
Advertisement
There’s no test that can diagnose psoriatic arthritis, but your provider might use tests to rule out other causes of your symptoms. They might use blood tests to check for infections. Imaging tests can take pictures of your joints to show damage or inflammation. You might need one or a few imaging tests, including:
Your healthcare provider will suggest treatments to manage your symptoms. Which treatments you’ll need depends on:
The most common treatments for psoriatic arthritis include:
It’s very rare to need surgery if you have psoriatic arthritis. If your joints are damaged or you’ve experienced bone loss, you might need an arthroplasty (joint replacement). Your provider or surgeon will tell you which type of surgery you’ll need and what to expect.
You should expect to manage your symptoms for a long time (maybe the rest of your life). Some people experience long periods of time between flares, but there’s no cure for psoriatic arthritis.
Advertisement
It can be frustrating when a flare happens suddenly. Eventually, you might learn to recognize the warning signs of a flare and start managing symptoms before they become more severe. Talk to a healthcare provider if you feel like your symptoms are getting worse or your current treatments aren’t managing them well enough.
Because experts don’t know what causes psoriatic arthritis, you can’t prevent it. You can lower your chances of developing all types of arthritis by:
Visit a healthcare provider if you notice new rashes or other symptoms on your skin or if you’re experiencing joint pain. Talk to your provider if your psoriatic arthritis symptoms are changing, flaring up more often or getting more severe.
Psoriatic arthritis and rheumatoid arthritis are different types of arthritis. They’re both autoimmune diseases.
Psoriatic arthritis is arthritis linked to psoriasis, a condition that affects your skin, fingernails and toenails. Rheumatoid arthritis is a type of arthritis that happens when your immune system attacks the tissue lining the joints on both sides of your body.
Neither condition is better or worse than the other. They’re both chronic (long-term) conditions you’ll need to manage for a long time. A healthcare provider will help you find treatments that manage your symptoms and reduce how much arthritis affects your life on a day-to-day basis.
Psoriatic arthritis symptoms can range from mild to severe. You might never experience severe symptoms. But there’s a chance your symptoms will vary between flares, often with seemingly no cause or reason. Psoriatic arthritis is a chronic (long-term) condition. In that sense, it’s serious — you’ll have to manage symptoms for a long time, maybe for the rest of your life. But between flares, you should be able to participate in all your usual activities.
It can be extremely frustrating to manage psoriatic arthritis. You might feel like you’re dealing with two conditions at the same time — the skin and nail symptoms of psoriasis and joint issues caused by arthritis. Your healthcare provider will help you find treatments that manage your symptoms during flares. They’ll also suggest ways you can keep your body healthy and strong to support your joints and skin.
Talk to your provider if it feels like your symptoms are changing, getting worse or flaring up more often. Listen to your body, and don’t hesitate to ask for adjustments in your treatment.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
From painful, swollen joints to irritated, scaly skin, psoriatic arthritis can complicate life. Cleveland Clinic is here to help you manage this condition.
