COVID-19 is an illness caused by the SARS-CoV-2 virus. It spreads through respiratory droplets. Symptoms include fever, cough, shortness of breath, runny or stuffy nose, body aches and more. COVID can cause mild to severe illness. Early treatment with antiviral medications can reduce your symptoms and your risk for severe illness.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
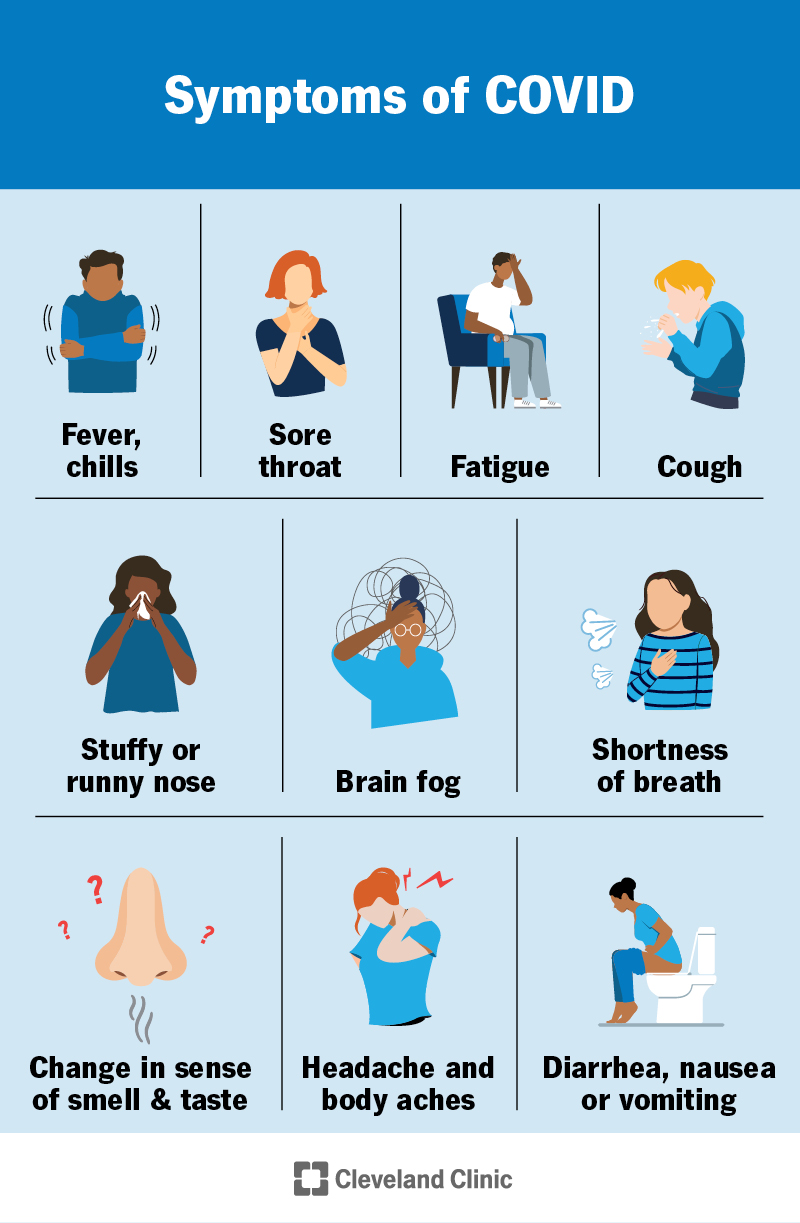
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/covid-symptoms)
COVID-19 is a respiratory illness caused by the SARS-CoV-2 virus, a type of coronavirus. Symptoms range from mild and cold-like to severe and life-threatening.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Coronaviruses have typically caused common colds. But in 2019, a new coronavirus, SARS-CoV-2, started infecting humans and causing severe illness. At the peak of the pandemic — when COVID was spreading around the world — tens of thousands of people were hospitalized every day in the U.S. alone. Millions of people have died.
Medical professionals’ understanding has grown a lot since the start of the pandemic. The virus itself keeps changing — we’ve gone through variants alpha, beta, gamma, delta and now omicron. Scientists have developed treatments and vaccines that have reduced the number of people ending up in the hospital.
But COVID isn’t “over.” It can still make you severely ill, cause symptoms that last months or years, and be fatal.
COVID symptoms include:
Some people have no symptoms but can still spread the virus.
SARS-CoV-2 virus causes COVID. It’s a type of coronavirus, a group of viruses that also cause common colds. But this isn’t the first time a coronavirus has caused serious illness. SARS, a severe respiratory disease that spread between 2002 and 2004, was also a coronavirus.
Advertisement
COVID spreads through respiratory droplets. This means you can get it from coughing, sneezing and talking. You might also get it from touching contaminated objects and surfaces.
You’re at an increased risk of being hospitalized with COVID-19 if you:
You’re also at an increased risk if you have:
COVID can cause serious complications, even if you don’t feel very sick. These include:
Healthcare providers diagnose COVID by swabbing your nose with a soft-tipped stick and testing it with a nucleic acid amplification test (NAAT), like a PCR test. You can also test at home with a rapid antigen test.
COVID can be treated with antiviral medications. These include nirmatrelvir/ritonavir (Paxlovid®), remdesivir (Veklury®) and molnupiravir (Lagevrio™). When taken within the first five days, antivirals can help you feel better and reduce your risk of severe illness and long COVID.
If you’re severely ill and hospitalized, your healthcare provider might treat you with:
Many people recover from symptoms like congestion, sore throat and cough in about two weeks. But tiredness, shortness of breath and other symptoms can linger for weeks or even months afterwards.
You can be contagious with COVID from a couple of days before your symptoms start to about eight to 10 days after.
If you have symptoms of COVID, talk to your provider early to see if you should take an antiviral. See your provider if your symptoms last longer than four weeks, especially if they aren’t improving.
Call 911 or get to an emergency room if you experience:
Advertisement
The outlook for COVID is different for everyone. Some people have only mild symptoms. Some get very sick and need to be hospitalized. Sometimes, your symptoms seem to get better and then get much worse. Always seek emergency medical attention for severe symptoms, no matter when they happen.
Over-the-counter medications can help ease some of the symptoms of COVID, though they won’t treat the virus itself. If your child has COVID, talk to their pediatrician before giving them medications to make sure they’re safe to take.
Making sure you’re up to date with a current COVID vaccine is the best way to reduce your risk of getting sick with COVID — and reduce your risk of severe illness if you do get sick. You’re also less likely to get long COVID if you’re vaccinated.
You can also reduce your risk by washing your hands frequently and wearing a mask when COVID is spreading. Be courteous and avoid being around others if you’re sick or might’ve been exposed to someone who’s sick.
If you have a compromised immune system, the monoclonal antibody medication pemivibart (Pemgarda™) might be an option. A provider gives it to you in an IV (through your vein) to reduce your risk of getting COVID (pre-exposure prophylaxis).
Advertisement
According to current CDC recommendations in the U.S., you should self-isolate until you’ve met both of the following criteria:
The beginnings of the COVID pandemic might seem far away at this point. Remembering things like elbow bumps and virtual birthday parties might even seem quaint. But COVID had a devastating effect on the world — and it seems to be here to stay. Vaccinations and antiviral medications can help reduce your risk of severe illness.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cold, flu or COVID-19? Cleveland Clinic will help you figure out what to do next.
