Your hepatic veins are located in your liver. They drain oxygen-poor blood from your liver into your inferior vena cava, which sends the blood back to your heart. You can keep your hepatic veins and the rest of your circulatory system healthy by limiting alcohol, avoiding tobacco and exercising regularly.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your hepatic veins are a group of blood vessels that drain blood from your liver into your inferior vena cava (IVC). Your IVC is a large vein that collects blood from your lower body and returns it to the top right chamber of your heart (right atrium).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The three major hepatic veins are your:
Your hepatic veins are an important part of your circulatory system. They’re responsible for draining oxygen-poor blood from your liver and carrying it to your inferior vena cava (IVC). This blood then flows through your heart and lungs and gains oxygen before your heart pumps it back out to your body.
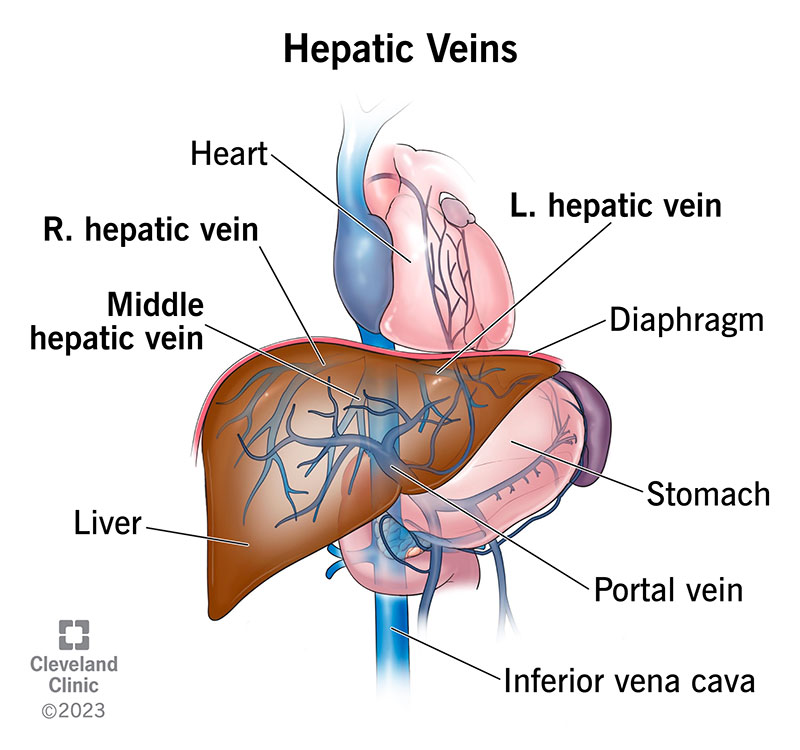
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/hepatic-veins.jpg)
Your hepatic veins are in your liver. They travel within and across your liver’s eight segments and mark the boundaries of its four anatomical sectors. Healthcare providers call these four areas your right anterior, right posterior, left medial and left lateral sectors.
Within your liver, your hepatic veins drain blood from your central veins. These are tiny blood vessels that collect blood from capillaries throughout your liver.
Your hepatic veins leave the back of your liver and immediately enter your inferior vena cava (IVC). They enter your IVC near your spine just below your diaphragm.
The right hepatic vein typically enters the IVC on its own, while the middle and left hepatic veins merge to form a common trunk before draining into the IVC. However, variations often occur.
Variations in your hepatic vein anatomy are harmless. But surgeons look for them before performing certain operations (like liver transplantation and liver resection).
Advertisement
There are many possible variations, including:
Hepatic veins have an average diameter of 15 millimeters.
Budd-Chiari syndrome is a condition that occurs when blood clots form in your hepatic veins. The clots narrow or block your veins, causing a backup of blood in your liver. This congestion disrupts the network of blood vessels in and around your liver. Possible complications include:
Symptoms of Budd-Chiari syndrome and its complications include:
Healthcare providers diagnose hepatic vein issues through a physical exam and one or more of the following tests:
Treatment includes medication to dissolve the blood clots (thrombolytic therapy) and procedures to help your blood flow better. Your provider will discuss specific treatment methods with you based on your diagnosis and individual needs.
Here are some tips for keeping your hepatic veins and all of your blood vessels working at their best:
Advertisement
No. Your hepatic veins and your portal vein are different blood vessels with opposite functions. Your portal vein, sometimes called your hepatic portal vein, carries blood into your liver. Meanwhile, your hepatic veins carry blood out of your liver.
Your portal vein is part of your portal venous system. This is a network of veins that drains blood from organs in your belly and sends it to your liver for processing.
Your hepatic veins aren’t part of that system. They carry blood that your liver has already processed. They deliver this blood to your inferior vena cava, which sends it directly to your heart.
Your hepatic veins are a crucial link between your liver and heart, allowing filtered (but oxygen-poor) blood to make its way back to your heart.
Talk to your healthcare provider if you’re concerned about the health of your liver or its blood vessels. They’re prepared to explain more about your anatomy and the lifestyle changes you can make to support your circulatory system.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a disease that’s affecting your liver, you want expert advice and care. At Cleveland Clinic, we’ll create a treatment plan that’s right for you.
