Eisenmenger syndrome is the development of pulmonary hypertension (high blood pressure in your lungs) due to an untreated congenital heart defect. Blood can’t flow normally through your lungs, leading to reduced oxygen in your blood. Nonsurgical treatments can reduce symptoms and manage complications, but there’s no cure.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Eisenmenger syndrome is a complication of certain untreated congenital heart defects. These defects make too much blood flow to your lungs, leading to raised pressure in your pulmonary arteries. Over time, the pressure gets so high that some blood reverses direction. Blood that should normally flow through your lungs instead goes back to your heart and out to your body.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
This means the blood that’s going out to your organs and tissues is low in oxygen. When your body can’t get enough oxygen, a wide range of symptoms and complications can develop. Some of these issues are life-threatening or fatal.
If you have Eisenmenger syndrome, you’ll need to work closely with a team of healthcare providers. They’ll help manage your condition. They’ll also help reduce symptoms so you can have a quality of life that’s meaningful to you.
Eisenmenger syndrome isn’t common in the U.S. and other developed countries. This is because healthcare providers usually diagnose and treat heart defects before they lead to serious problems. But this condition remains common in many low- and middle-income countries with limited access to healthcare.
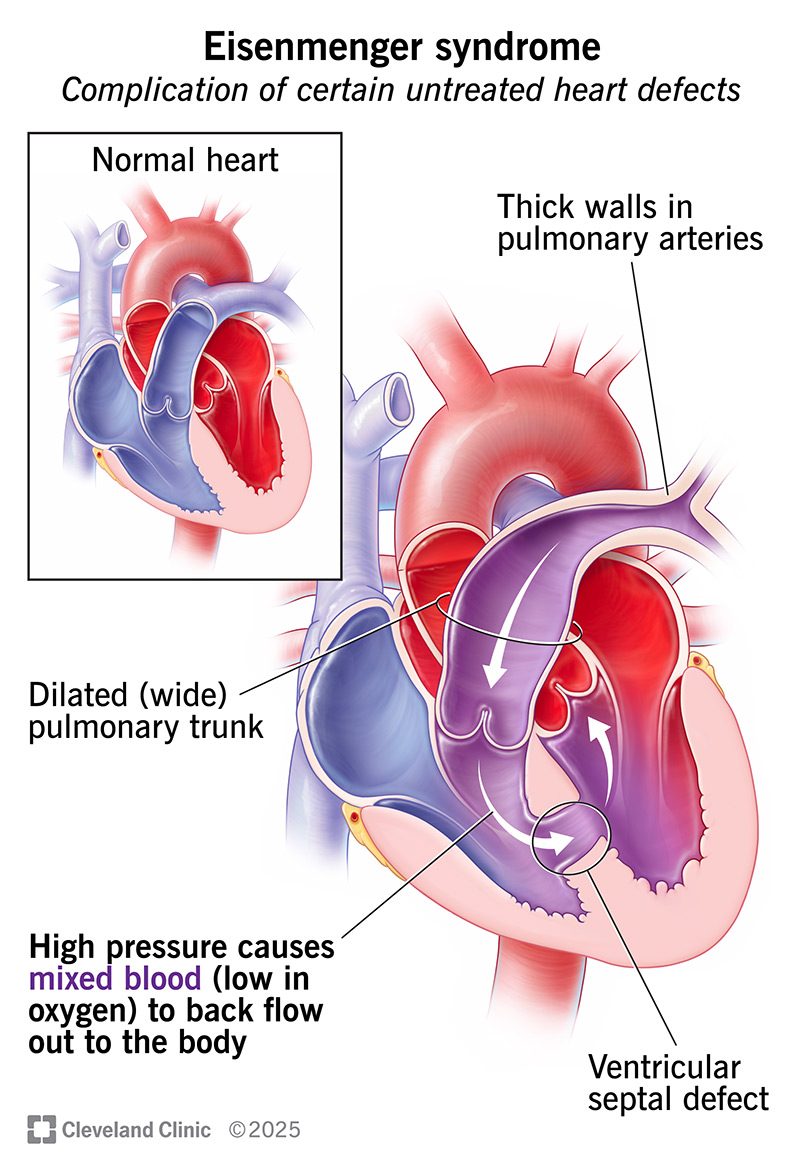
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/17921-eisenmenger-syndrome)
Eisenmenger syndrome causes symptoms of hypoxemia, or low blood oxygen levels. You might feel short of breath when you’re moving around. You may also notice a blue tint to your skin, called cyanosis. This can appear on your cheeks, lips, gums, hands and/or feet. Cyanosis can be harder to notice if you have darker skin.
You’ll likely also have symptoms of pulmonary arterial hypertension, which include:
Advertisement
Eisenmenger symptoms usually develop in adolescence or adulthood. But they may appear much sooner, including in early childhood.
An unrepaired hole between your heart chambers or your aorta and pulmonary artery causes Eisenmenger syndrome. The hole creates a left-to-right shunt, or an abnormal passage for blood flow to your lungs. Over time, this increased blood flow damages arteries in your lungs and raises the pressure in them, leading to pulmonary arterial hypertension (PAH).
PAH makes it hard for blood to flow through your lungs as it should because the pressure is high. Eventually, your blood faces so much resistance that it starts to reverse direction. This causes some blood to flow back to your heart, rather than flowing through your lungs. Now, blood flows from right to left through the hole or in both directions. This reversed (right-to-left) shunt is a hallmark of Eisenmenger syndrome.
Congenital heart defects that can cause Eisenmenger syndrome include:
Eisenmenger syndrome affects many different parts of your body. A common complication is that your body makes more red blood cells. This is called secondary erythrocytosis. It’s your body trying to compensate for low levels of oxygen in your blood.
Other complications include:
Pregnancy is very dangerous if you have Eisenmenger syndrome. There’s a high risk of serious complications, including maternal or fetal death.
If there’s a chance you could become pregnant, talk to your healthcare provider. They’ll advise you on contraception. They’ll also help you understand other options for growing your family, like adoption and gestational surrogacy.
A physical exam, along with your medical history, might make your healthcare provider suspect Eisenmenger syndrome. Then, they’ll run tests to see what’s going on.
Advertisement
Tests you may need include:
Some of these tests check your heart function and blood flow through your heart and lungs. Others help diagnose complications, like a high red blood cell count.
Diagnosing Eisenmenger syndrome frequently involves some type of imaging test to determine the location of the shunt (where the blood goes the wrong direction). It may also involve a heart catheterization, which is the gold standard to determine how much blood is going in the wrong direction and what the pressure is in your lungs.
Treatment for Eisenmenger syndrome involves medicines to help blood flow better through your lungs and reduce your symptoms. Providers also give you treatments to prevent or manage complications. Surgery can’t repair the issue, but organ transplants are an option for some people.
Possible treatments include:
Advertisement
Providers can’t repair the heart defect that’s causing Eisenmenger syndrome. Up until now, your body has tried to adapt to the flow issues in your heart and lungs. Your body can’t undo that work fast enough if your provider fixes the defect. So, surgical repair can lead to serious complications. But researchers continue to look into new approaches that might help people one day.
There’s a lot you can do in your daily life to help manage Eisenmenger syndrome. Talk to your provider for advice tailored to your needs. They may recommend that you:
You’ll need to see a cardiologist and pulmonologist for life. They’ll tell you when to come in for appointments. You may also need to see other specialists, like a hematologist, depending on the complications that develop.
If possible, seek care at a large medical center where doctors have experience in treating adult congenital heart disease and pulmonary hypertension.
Eisenmenger syndrome typically shortens a person’s lifespan. It’s sometimes fatal in childhood. But many people live to early adulthood or even middle age. How long you live depends on many factors, including the type of heart defect you were born with and any other conditions you have.
Advertisement
Your healthcare providers can give you the most accurate prognosis. In general, research shows:
The most common causes of death for people with Eisenmenger syndrome are:
It’s a good idea to talk to your providers and a lawyer about advanced directives. These legal documents can help ensure your wishes for medical care, including at the end of life, are carried out. You may also want to learn about palliative care options. It can be hard to think about these things. But such planning can help both you and your loved ones in the future.
Eisenmenger syndrome isn’t an easy diagnosis to hear. Your providers understand this. They’ll be with you each step of the way as you learn more about this condition and your treatment options.
During this time, it can help to build a support system around you. That might be friends or family. Or it might be a community of people who have heart or lung disease. They can offer advice and a listening ear.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you were diagnosed as a child or later in life, Cleveland Clinic is here to treat your adult congenital heart disease.
