Epididymitis is inflammation in the sperm-carrying tube at the back of your testicle. The swelling can cause intense pain in or around your testicle and scrotum. It can occur at any age. But it happens most often in people between the ages of 14 and 35.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
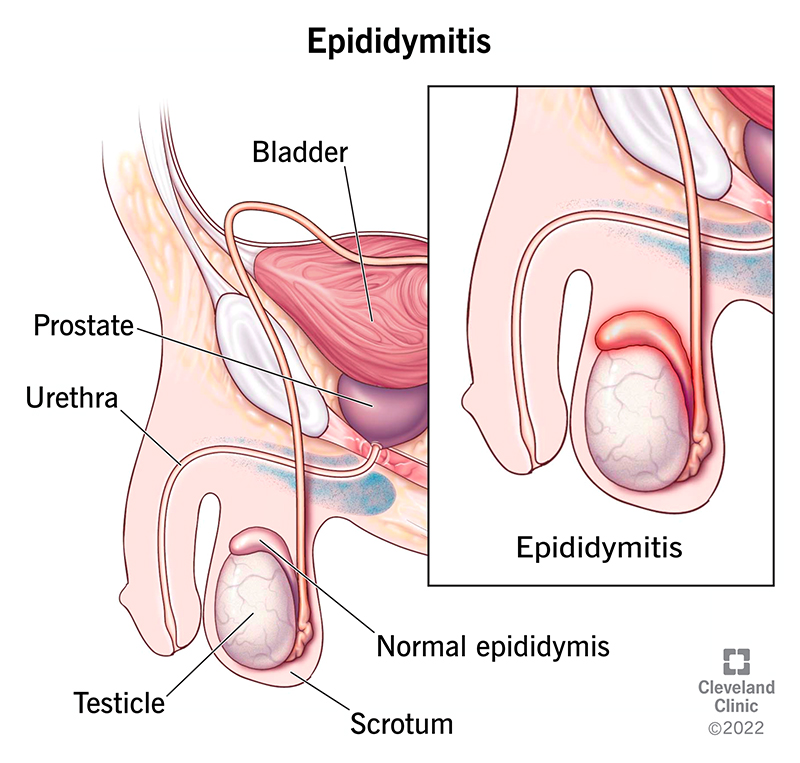
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/epididymitis)
Epididymitis (up-uh-DID-uh-MI-tis) is inflammation of your epididymis (ep-uh-DID-uh-miss) that causes discomfort or pain in your scrotum, testicle or epididymis. Your epididymis is a coiled tube at the back of your testicle — most people have one behind each testicle (plural epididymides). It stores and carries sperm.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Inflammation anywhere in your body can be painful and uncomfortable. It can be even more distressing when it affects a sensitive area. But inflammation is your body’s way of telling you that something’s wrong, and you should talk to a healthcare provider. They’ll do their best to identify what’s causing your pain, treat you promptly and put your mind at ease.
There are two general types of epididymitis:
There are about 600,000 cases of epididymitis in the United States each year.
Epididymitis symptoms may include:
A bacterial infection is the most common cause of acute epididymitis. If you’re under 35 years of age, sexually transmitted infections (STIs) — such as gonorrhea or chlamydia — are the most common cause of epididymitis.
Advertisement
If you’re older than 35, the most common cause of epididymitis is the backflow of infected pee (urine) down your ejaculatory tract to the epididymis. The most common bacteria that associates with this is E. coli. Men who have sex with men also have an increased risk of epididymitis from exposure to gastrointestinal bacteria, such as E. coli.
Other infections, including the mumps virus and, rarely, tuberculosis, can also cause epididymitis.
Other less common causes of epididymis include:
Yes, you can get epididymitis through nonsexually transmitted infections. For example, prostate infections and UTIs can spread to your epididymis.
Yes, epididymitis can spread through sexual contact. While healthcare providers don’t categorize it as an STI, it’s still a common symptom of many STIs, including chlamydia and gonorrhea.
Males develop epididymitis. It can occur at any age.
Without treatment, epididymitis can cause complications, like an abscess in your scrotum. Your scrotal skin can also open up or break because of swelling and infection.
In rare cases, epididymitis can cause male infertility problems. You can help prevent these complications by seeking treatment as soon as you notice symptoms.
A healthcare provider will ask you questions about your symptoms and perform a physical examination of your scrotum to look for a tender area or lump. They may also order tests, including:
Epididymitis treatment depends on the cause.
If bacteria cause epididymitis, treatment involves antibiotics. The most common medications include:
Most people need to take antibiotics for about one to two weeks. In rare cases, you may need a prolonged course of antibiotics.
If tuberculosis causes epididymitis, a healthcare provider may prescribe:
Advertisement
Most people need to take antituberculosis medications for six to nine months.
In severe cases, a surgeon may need to remove one or both of your epididymides (epididymectomy) or testicles (orchiectomy).
If the arrhythmia medication amiodarone causes epididymitis, a healthcare provider may reduce your dosage or prescribe another medication. Talk to a provider before you adjust or stop taking amiodarone.
Epididymitis treatment varies for non-infection causes. A healthcare provider will talk to you about how to stay comfortable.
Bacteria causes most cases of epididymitis. Bacterial epididymitis cases won’t go away on their own. It’s important to talk to a healthcare provider as soon as you notice symptoms to get proper treatment and avoid further complications.
Ejaculating won’t make epididymitis worse. But it can make the pain more intense for some people. You shouldn’t have sexual intercourse with anyone until a healthcare provider says it’s OK. It’s also best to avoid masturbation until you complete your treatment.
You can’t self-treat most cases of epididymitis. It’s important to talk to a healthcare provider for an official diagnosis and treatment. But you can help relieve epididymitis symptoms by:
Advertisement
Not everyone can take NSAIDS, so talk to a healthcare provider before you take them.
It depends on what causes epididymitis.
In most cases of bacterial infection, you should start to feel better a few days after starting antibiotics. However, swelling can take several weeks to improve. It’s possible to experience discomfort or swelling for weeks or even months after you finish your course of antibiotics.
Tuberculosis epididymitis may take up to nine months for you to heal with medications.
If amiodarone causes epididymitis, you should start to feel better shortly after you reduce your dosage or stop taking it.
In extremely rare circumstances, if a surgeon removes your epididymides or testicles, you may experience worsening pain immediately after surgery due to swelling. It can take several weeks to feel better after surgery. But that doesn’t mean the surgery was ineffective.
In most cases of epididymitis, a healthcare provider will prescribe antibiotics to treat the infection and ease your symptoms. They’ll also give you advice on how to relieve discomfort at home.
Advertisement
While epididymitis can be painful, it usually doesn’t cause any long-term problems, especially with early treatment. Be sure to talk to a healthcare provider as soon as you notice symptoms.
Most people who get treatment for epididymitis start to feel better after about three days. But your symptoms may continue for weeks or even months after treatment.
It’s important to finish your full course of antibiotics, even if you start to feel better. If you don’t, epididymitis may return and be harder to treat.
If symptoms return, follow up with a healthcare provider. They can rule out other conditions that affect your testicle. Although testicular cancer rarely causes pain or swelling, routine follow-ups with a provider are important to rule out cancer or conditions.
You can help reduce your risk of epididymitis by:
Call a healthcare provider if you develop any symptoms of epididymitis. If they conclude that your infection is due to an STI, be sure to let your recent sexual partners know so they can schedule an appointment with a provider and get treatment.
Head to your nearest emergency room or call 911 (or your local emergency number) if you develop sudden or severe testicular pain.
If a healthcare provider diagnoses you with epididymitis, you’ll want to learn all you can about your outlook and treatment options. Here are some questions you may want to ask a provider:
The following conditions share similar symptoms as epididymitis:
Epididymitis refers to inflammation of the tube at the back of your testicle. Orchitis is when your testicle itself swells. These conditions sometimes occur at the same time. When this happens, healthcare providers call it epididymo-orchitis.
Discomfort or pain in or around your testicles might not be something that’s easy to talk about. But even though it might be embarrassing, it’s important to get it checked out by a healthcare provider. Providers are caring and professional, and your health is important to them. But so is your comfort. They’ll do their best to make your visit as stress-free as possible. Remember to take all medications exactly as they prescribe and to follow their recommendations to ensure a successful recovery.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a condition that’s affecting your urinary system, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
