Pelvic floor dysfunction is the inability to correctly relax and coordinate your pelvic floor muscles to poop. Symptoms include constipation, straining to poop, having urine (pee) or stool leakage and experiencing a frequent need to pee. Treatments include biofeedback, pelvic floor physical therapy and medications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
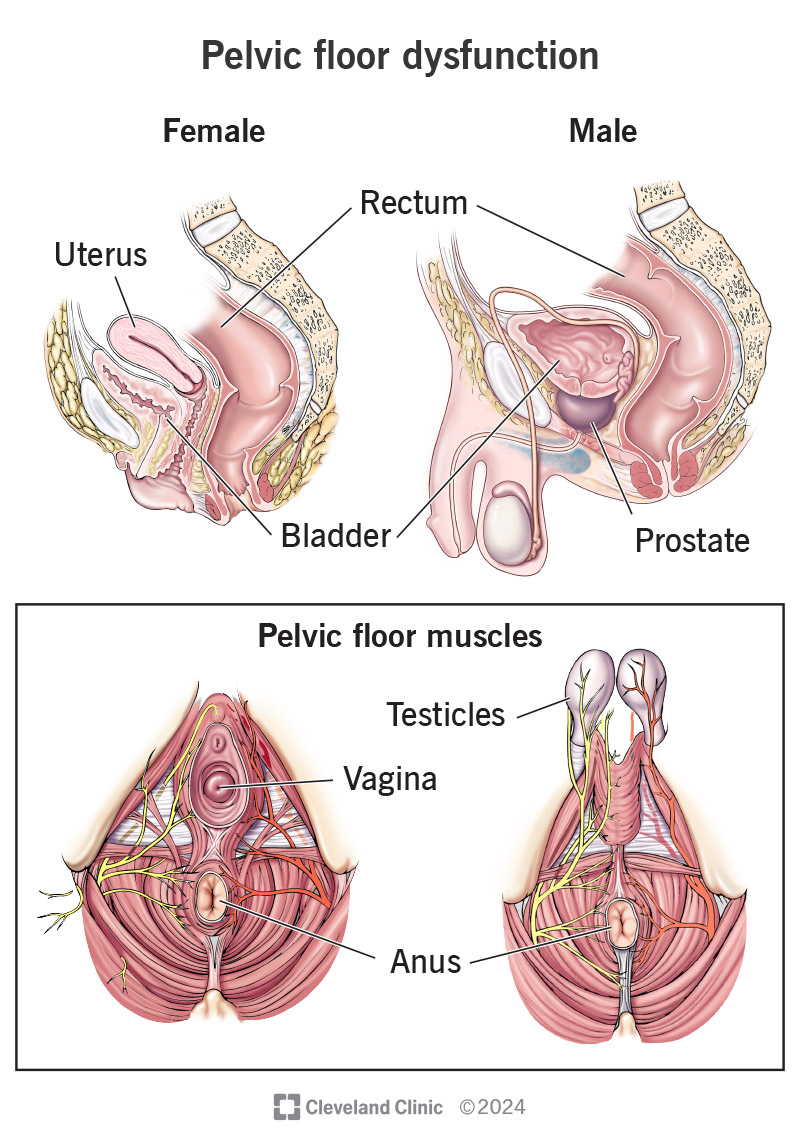
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/Images/org/health/articles/14459-pelvic-floor-dysfunction.jpg)
Pelvic floor dysfunction is a common condition where you can’t correctly relax and coordinate the muscles in your pelvic floor to urinate (pee) or have a bowel movement (poop). Think of your pelvis as being home to organs like your bladder, uterus, prostate and rectum. Your pelvic floor muscles are the home’s foundation. They’re the support structure keeping everything in place.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Normally, you’re able to go to the bathroom without issue because your body tightens and relaxes your pelvic floor muscles. This is just like any other muscular action, like tightening your biceps when you lift a heavy box or clenching your fist.
But if you have pelvic floor dysfunction, your body keeps tightening these muscles instead of relaxing them. This tension means you may have:
If you’re female, pelvic floor dysfunction may also cause pain during intercourse. If you’re male, you may have problems getting or keeping an erection (erectile dysfunction).
The following signs and symptoms can let you know you might have a pelvic floor issue:
Advertisement
Experts don’t know the exact cause of pelvic floor dysfunction. But, a few known factors may play a role. These include:
Pelvic floor dysfunction can exist alongside (and be mistaken for) many other conditions, including:
A healthcare provider will usually start by asking about your symptoms and taking a medical history. Your provider may ask:
If you’re female, they may ask about prior pregnancies and if you’re experiencing pain during sex.
Your provider may do a physical exam to test how well you can control your pelvic floor muscles. Using their hands, your provider will check for spasms, knots or weakness in these muscles. Your provider will also perform a rectal exam and (if you’re female) a pelvic exam.
You may also need other tests, including:
Advertisement
Healthcare providers can treat pelvic floor dysfunction without surgery. Treatments include:
Advertisement
It may take a few months of physical therapy sessions to notice symptom improvements. But most people do eventually notice a difference. Biofeedback helps over three-quarters of people with pelvic floor dysfunction gain better muscle control.
Unfortunately, no. Pelvic floor dysfunction symptoms (like an overactive bladder) typically stay or become worse if they’re not treated. Pelvic floor dysfunction is treatable, but you’ll need to see a provider who can diagnose and treat the symptoms.
Not giving up is the most important part of living with pelvic floor dysfunction. It can take several months of routine bowel or urinary medications and pelvic floor physical therapy before symptoms start to improve. But most people who stick to their care plan notice improvements.
In the meantime:
Advertisement
Although pelvic floor dysfunction is common, it can be embarrassing to discuss your symptoms — especially difficulty peeing or pooping. But having a conversation with your provider about your symptoms gets you one step closer to relief. Many pelvic floor dysfunction symptoms are easy to treat. But you have to reach out. Remember, the more open and honest you are with your provider, the better your treatment will be.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
