An anal fissure is a crack or split in the tissues that line your anal canal. Trauma causes the lining to tear, causing acute pain and bleeding. Most fissures heal with self-care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
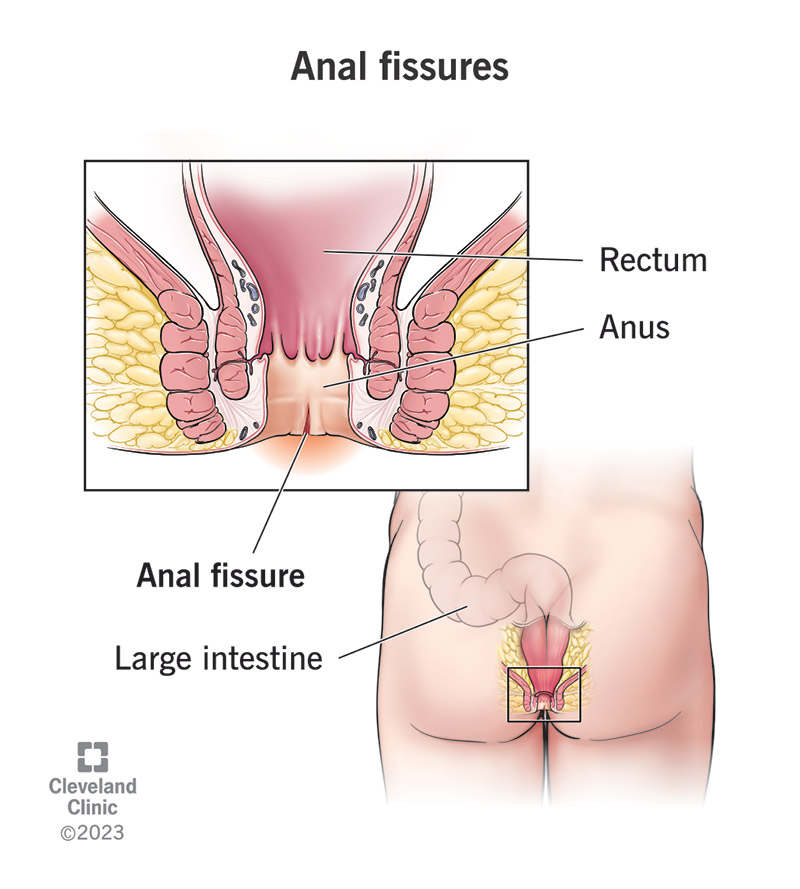
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/13177-anal-fissures)
An anal fissure is a crack or tear in the lining of your anal canal. It’s a common cause of anal pain and rectal bleeding, especially during bowel movements (pooping).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Anal trauma usually causes a fissure, especially from straining to pass hard stools. Anal fissures can occur suddenly or gradually. They can also heal quickly or slowly.
Anal fissures are very common, especially in infants and pregnant women. About half of people with anal fissures get them before they turn 40.
The most common symptoms are:
Some people may also have:
Most people — but not all — feel pain with an anal fissure. They feel it most when pooping, but it can last for minutes to several hours after. They describe it as sharp, tearing, cutting or burning. Some people find that the pain radiates to their buttocks, upper thighs or lower back.
Hemorrhoids and anal fissures have similar symptoms and causes, and it’s easy to mistake one for the other. Both can happen when you strain too much to poop, and both can cause rectal bleeding, anal pain and anal itching.
While hemorrhoids are more common, anal fissures are more commonly the cause of anal pain. Hemorrhoids don’t always cause pain, but 90% of fissures do. However, the pain from a fissure usually occurs in episodes, while hemorrhoid pain can be constant.
Advertisement
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_bl79f9tu/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
Learn the difference between an anal fissure and an anal fistula.
Trauma — like stretching and straining — causes your anal lining to tear. But preexisting conditions can also play a role. This has to do with the anatomy of your anus (butthole), which is really the last few centimeters of the long, muscular tube known as your large intestine.
Toward the end of your anus, where it opens to the outside, the skin is more like the skin on the outside of your body. But in the upper portion, where fissures usually happen, your anus is lined with the same soft mucosa as the rest of your large intestine.
This mucous lining is thinner and more delicate than normal skin, making it easier to tear. This is especially true for babies, who often get anal fissures. It can also become inflamed by injury or disease. Long-term (chronic) inflammation can weaken the tissues.
Your anus is surrounded by two circular muscles that help control your bowel movements (your anal sphincters). If these muscles are too tight, they can add tension to your anal lining, making it easier to tear and even reducing blood flow to the tissues.
Many anal fissures heal by themselves in a few weeks, but complications can develop when they don’t. These are called chronic anal fissures. Instead of healing, they continue to reinforce themselves in a vicious cycle, leaving a persistent wound.
Pain and muscle clenching can cause your anal muscles to tighten and spasm. Muscle tension and anal spasms pull the fissure apart and reduce blood flow to the tissues. This makes it harder for it to heal, and also more painful, causing more tension.
If anal fissures go on too long without healing, they can lead to further complications, such as:
A healthcare provider will ask you about your symptoms, then try to see the fissure. You’ll lie on your belly or on your side while they gently separate your buttocks. If this is too painful, they don’t have to go further. They can safely assume that you have an anal fissure.
But if you can tolerate an exam, they’ll try to see the fissure so that they can rule out other possible causes for your symptoms. They might gently insert a lubricated gloved finger to open your anus, noticing any tenderness or muscle spasms. This is a digital rectal exam.
Advertisement
Most do. These are acute anal fissures (temporary). They might not need any treatment at all, beyond self-care. Or you might only need a prescription cream for temporary pain relief, like lidocaine. But if your fissure hasn’t healed after several weeks, it needs treatment.
Most anal fissures heal within a few days to weeks. A chronic anal fissure lasts more than eight weeks. If you’re in treatment for a chronic anal fissure, it may take another six to 12 weeks for the treatment to work and the fissure to finally heal.
When you have a chronic anal fissure — one that has lasted more than eight weeks — medical treatment focuses on relaxing the anal sphincter muscles that surround your anal canal. This should allow the fissure to begin to close and help restore blood flow to the tissues.
Medications for anal fissures include:
Advertisement
If your anal fissure won’t heal with medication, or it comes back after healing, you might need a minor medical procedure to end the cycle. Medications have mixed results for chronic anal fissures, but surgery, if it comes to it, has a 90% success rate.
The procedure is called an internal sphincterotomy. While you’re asleep under sedation, a colorectal surgeon makes a small cut into your anal sphincter muscle to release tension permanently. After you wake up, you can go home the same day.
If you have a chronic condition that affects your anus, whether it’s a disease, trouble with pooping or unexplained pain, see a healthcare provider about it. Treating these conditions sooner can prevent complications like anal fissures from developing or returning.
Follow these tips to stay regular and prevent constipation before it becomes a medical problem.
Most anal fissures will heal on their own, but you can help the process along with a little self-care. Here’s some advice:
Advertisement
It might help to:
Anal fissures are common, and not normally dangerous, but they can hurt a lot. Most anal fissures heal in a few days to weeks with a little self-care. But some anal fissures are more complicated and may resist healing. If you have a chronic fissure, don’t hesitate to seek medical treatment. A healthcare provider will work with you to bring you relief.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have issues with your digestive system, you need a team of experts you can trust. Our gastroenterology specialists at Cleveland Clinic can help.
