Your pelvic floor muscles help stabilize your core while assisting with bodily functions, like pooping, peeing and having sex. They can weaken over time due to injury and aging. This may lead to conditions like incontinence or pelvic organ prolapse. Exercising your pelvic floor muscles may help fix these issues.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
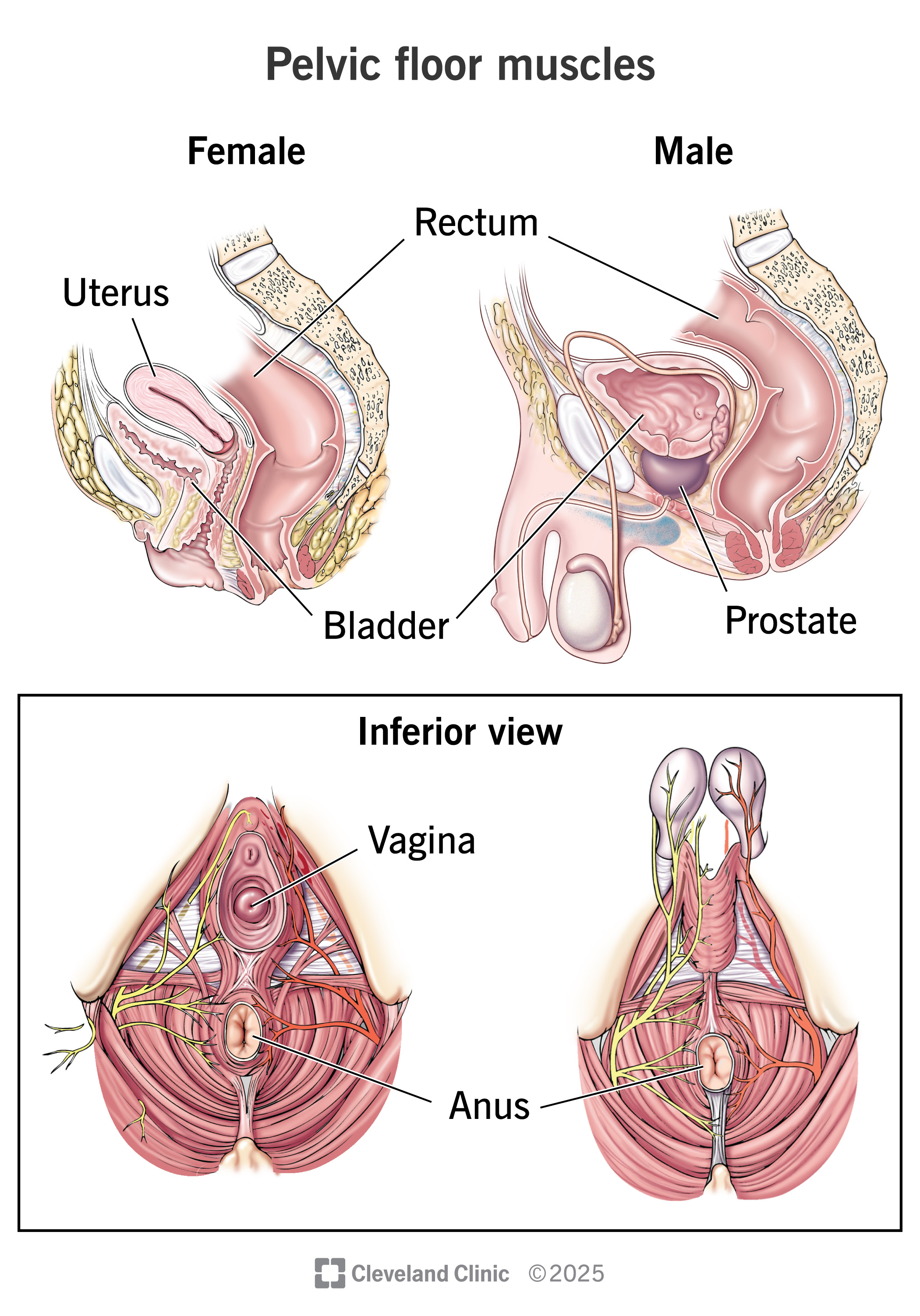
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22729-pelvic-floor-muscles)
Your pelvic floor muscles support organs in your pelvis. These include your bladder, bowel and internal reproductive organs. You can think of your pelvic floor muscles like a bowl or sling that holds these organs in place. The muscles also assist with bodily functions like peeing, pooping and sex.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You may not think twice about the muscles in your pelvis until you face issues with pee and poop control. That’s because these muscles often do their job automatically. The good news is that specialized physical therapy (like Kegels) can help restore your pelvic floor muscle function.
Your pelvic floor muscles:
Your pelvic floor muscles hold the major organs in your pelvis in place and protect them. Pelvic floor muscles support your:
In females, they also support the vagina and uterus. In males, they also hold the prostate in place.
Advertisement
Squeezing your pelvic muscles narrows your urethra and anus so waste material can’t escape. Relaxing these muscles widens these passages so you can pee, poop or fart.
Healthy pelvic floor muscles can squeeze and relax automatically. You can also control these muscles deliberately, much like flexing a bicep.
Your pelvic floor muscles stretch from your pubic bone in the front of your body to your tailbone in the back. The muscles extend outward on both sitting bones on the right and left sides of your pelvis. Several pelvic floor muscles intertwine to form a single sheet of layered muscle with openings.
You can feel where your pelvic floor muscles are by squeezing these three openings:
In each case, you should feel muscles inside your pelvis pull inward and upward. These are your pelvic floor muscles.
Your pelvic floor muscles form the base of a group of muscles known as your core. Your core muscles include your:
Together, these muscles attach to your pelvis and spine. They create stability throughout your body’s center. This allows you to maintain your posture and balance and move effectively.
You have 14 pelvic floor muscles that intertwine and layer together to form a sheet of muscle.
The two main pelvic floor muscles include:
Pelvic floor dysfunction is a group of conditions in which you can’t properly relax and/or use your pelvic floor muscles. The muscles may be too loose and weak or too tight.
Pelvic floor muscles can weaken from injury or trauma, including childbirth and surgery. They can also weaken during pregnancy or from overuse (like repeated heavy lifting or chronic coughing).
Weak pelvic floor muscles can lead to conditions like:
Advertisement
When these muscles are too tight, healthcare providers call it hypertonic pelvic floor. Researchers haven’t studied hypertonic pelvic floor as much as weakened pelvic muscles. But having tight pelvic muscles may lead to issues like:
If you can control when you release pee, poop and gas, there’s a good chance that your pelvic floor muscles are strong and healthy. But certain things, like pregnancy or prostate surgery, can affect previously strong pelvic floor muscles.
It’s a good idea to talk to a healthcare provider if you’re concerned about your pelvic floor muscles. They can walk you through pelvic floor exercises.
Remember that the goal is balance. Your pelvic floor muscles should be strong enough to stabilize your core and secure your organs. But they also need to be flexible enough to stretch and relax.
Your pelvic floor muscles are critical to your health and quality of life. Keeping these muscles strong and flexible can help prevent issues like incontinence and prolapse. Like any muscle, it takes time to build them up, so consistency with pelvic floor exercises is key. Don’t hesitate to ask a healthcare provider for guidance. They’re available to help.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.
