Thyroid cancer develops in your thyroid gland, a part of your endocrine system. Your thyroid gland produces hormones that regulate body temperature, heart rate and metabolism. Most thyroid cancers are highly curable. Treatments include surgery, chemotherapy, radiation, hormone therapy and radioiodine therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
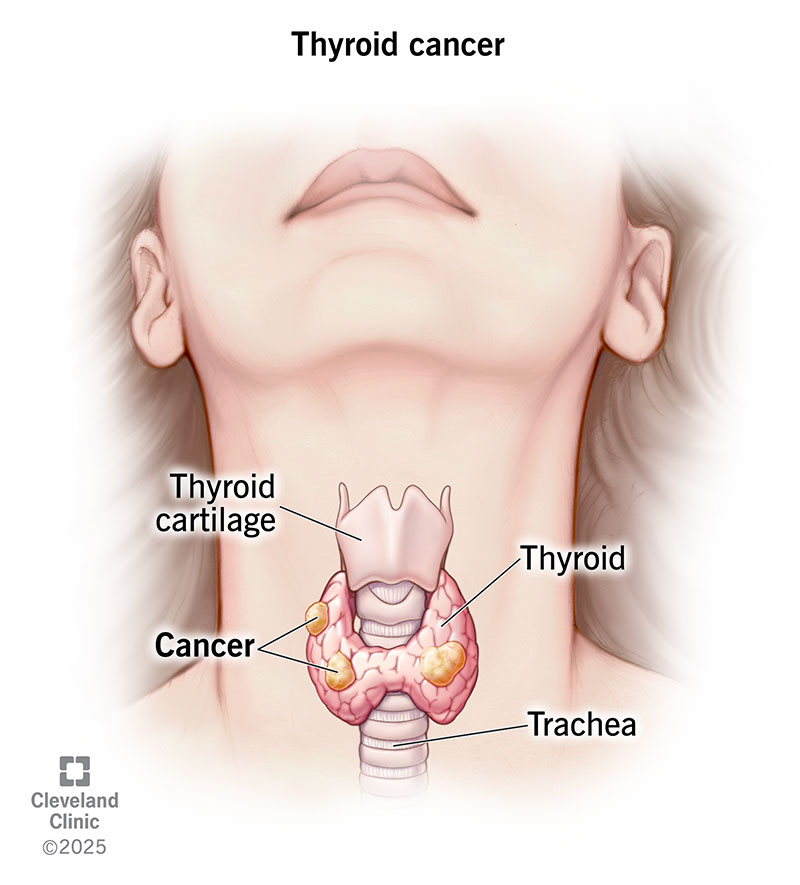
Thyroid cancer develops in your thyroid, a small, butterfly-shaped gland at the base of your neck. This gland produces hormones that regulate your metabolism (how your body uses energy). Thyroid hormones also help control your body temperature, blood pressure and heart rate. Thyroid cancer, a type of endocrine cancer, is generally highly treatable, with an excellent cure rate.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Close to 53,000 Americans receive a thyroid cancer diagnosis every year. Treatments for most thyroid cancers are very successful. Still, about 2,000 people die from the disease every year.
Women are three times more likely to get thyroid cancer compared to men. The disease is commonly diagnosed in women in their 40s and 50s and men in their 60s and 70s. Even children can develop the disease.
Healthcare providers classify thyroid cancer based on the type of cells from which the cancer grows. Types of thyroid cancer include:
Advertisement
Healthcare providers use a staging system to determine if and how far thyroid cancer has spread. Generally, when cancer cells in your thyroid metastasize, they spread to your nearby structures and lymph nodes first. After that, the cancer can spread to distant lymph nodes, organs and bones.
Thyroid cancer stages range from 1 (I) to 4 (IV). In simple terms, the higher the number, the more the cancer has spread. To learn more about cancer staging and how it applies to your specific diagnosis, talk to your healthcare provider.
You or your healthcare provider might feel a lump or growth in your neck called a thyroid nodule. Don’t panic if you have a thyroid nodule. Most nodules are benign (not cancer). Only about 3 out of 20 thyroid nodules turn out to be cancerous (malignant).
Other thyroid cancer symptoms include:
If you have thyroid cancer that has spread (metastasized) to other areas of your body, you may experience symptoms such as:
Experts aren’t sure why some cells become cancerous (malignant) and attack your thyroid. Certain factors, such as radiation exposure, a diet low in iodine and faulty genes can increase the risk. Other risk factors include:
If you have an enlarged thyroid nodule or other signs of thyroid cancer, your healthcare provider may order one or more of these tests:
Advertisement
Treatments for thyroid cancer depend on the tumor size and whether the cancer has spread. Treatments include:
Advertisement
Thyroid cancer can spread (metastasize) to other parts of your body, such as your liver, lungs or bones. Detecting and treating thyroid cancer in the early stages reduces your risk for metastasis.
Thyroid cancer can recur (come back), even after treatment. Because thyroid cancer grows slowly, it could take up to 20 years to come back. Recurrence happens in up to 30% of thyroid cancer cases.
Overall, thyroid cancer prognosis (outlook) is positive. But it’s important to know that after thyroid surgery or treatments, your body still needs thyroid hormones to function. You’ll need thyroid hormone replacement therapy for life. Synthetic thyroid hormones, such as levothyroxine (Synthroid®), take over for the thyroid hormones that your body no longer naturally produces.
Thyroid cancer is the second most common cancer diagnosed in pregnancy (breast cancer is the first). Approximately 10% of thyroid cancers develop during pregnancy or within the first year after childbirth. Experts believe fluctuating hormone levels during pregnancy may trigger the cancer.
If you receive a thyroid cancer diagnosis during pregnancy, your healthcare provider can discuss treatment options. Depending on the cancer type and severity, your provider may recommend delaying treatment until after you deliver your baby. If treatment can’t wait, most people can safely undergo surgery to remove the cancerous gland. You shouldn’t have radioactive diagnostic tests or treatments when you’re pregnant or breastfeeding.
Advertisement
Recovery depends on several factors, including your age, the size and stage of your thyroid tumor, and what type of treatment you received. Talk to your healthcare provider about what to expect during and after your thyroid cancer treatment.
Eight out of 10 people who have thyroid cancer develop the papillary type. Papillary thyroid cancer has a five-year survival rate of almost 100% when the cancer is in their gland (localized). Even when the cancer spreads (metastasizes), the survival rate is close to 80%. This rate means that, on average, you’re about 80% as likely to live for at least five years after diagnosis as someone who doesn’t have metastatic papillary thyroid cancer.
Five-year survival rates for other thyroid cancer types include:
Yes, most thyroid cancers are curable with treatment, especially if the cancer cells haven’t spread to distant parts of your body. If treatment doesn’t fully cure thyroid cancer, your healthcare provider can design a treatment plan to destroy as much of the tumor as possible and prevent it from growing back or spreading.
Many people develop thyroid cancer for no known reason, so prevention isn’t really possible. But if you know you’re at risk for thyroid cancer, you may be able to take steps to prevent it. These include:
You should call your healthcare provider if you have thyroid cancer and you experience:
If you have thyroid cancer, you may want to ask your healthcare provider:
Receiving a cancer diagnosis is unsettling, regardless of the type. Fortunately, most thyroid cancers respond extremely well to treatment. Your healthcare provider can discuss the best treatment option for the type of thyroid cancer you have. After treatment, you may need to take synthetic thyroid hormones for life. These hormones support vital body functions. They usually don’t cause any significant side effects, but you’ll have regular checkups to monitor your health.
Hearing you have cancer can be scary. But most thyroid cancer is treatable, and the providers at Cleveland Clinic are here to help.

Last reviewed on 10/24/2022.
Learn more about the Health Library and our editorial process.