Medullary thyroid cancer (MTC) forms in the inside of your thyroid gland, which is called the medulla. It’s the rarest type of thyroid cancer. While most cases are sporadic (random), about 25% of cases are linked to an inherited condition called multiple endocrine neoplasia type 2.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
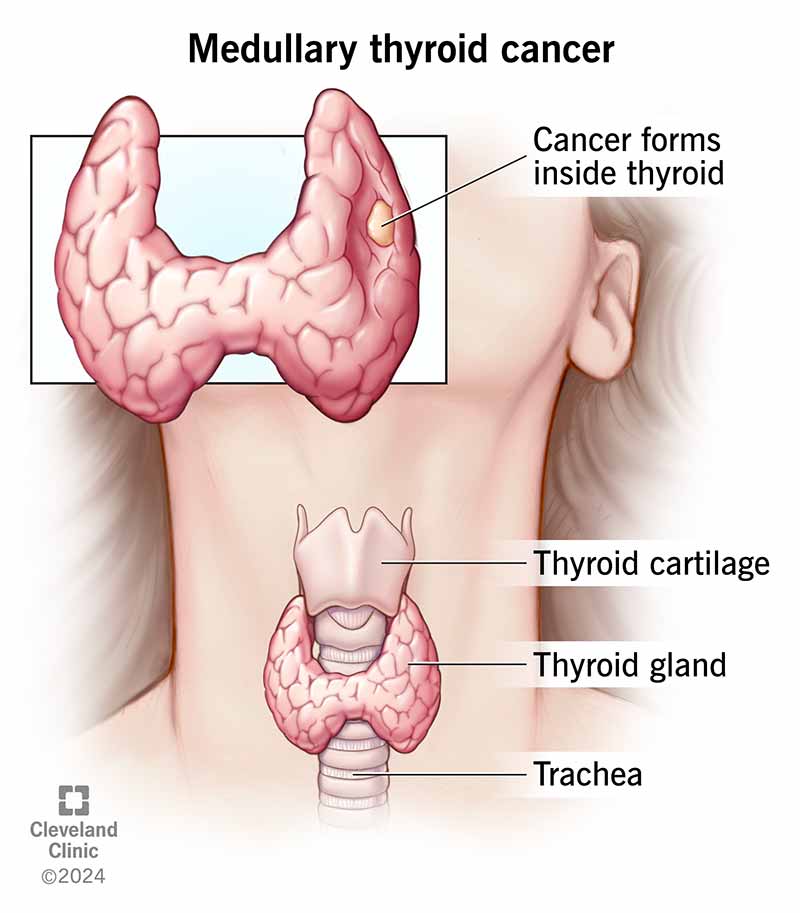
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/22873-medullary-thyroid-cancer-mtc)
Medullary thyroid cancer (MTC) is cancer that forms inside your thyroid gland. The inside is called the medulla. It contains special cells called parafollicular C cells that make calcitonin, a hormone. MTC happens when the C cells grow out of control.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hearing you might have cancer can leave you with many questions and worries, especially when it’s rare. Know that your healthcare team will be by your side along the way. Several therapies can help treat MTC.
Thyroid cancer, in general, is fairly common. But medullary thyroid cancer, specifically, is rare. Approximately 4% to 10% of all thyroid cancers in the United States are MTC. About 1,000 people receive an MTC diagnosis each year in the U.S.
Symptoms of medullary thyroid cancer include:
In rare cases, an enlarged thyroid nodule can cause:
In some cases, people have MTC for a long time before they notice symptoms. This is because the tumor remains small.
About 75% of medullary thyroid cancer (MTC) cases (3 in 4) are sporadic. This means it happens in people who don’t have a family history of MTC. Scientists haven’t yet figured out the exact cause of sporadic MTC. But 40% to 50% of people with sporadic MTC have acquired mutations in the RET gene. This means you develop the genetic mutation later in life — you aren’t born with it.
Advertisement
In up to 25% of cases (1 in 4), MTC is due to an inherited condition called multiple endocrine neoplasia type 2 (MEN2). There are different subtypes of MEN2, including:
There’s also a subvariant of MEN2B called familial medullary thyroid cancer (FMTC). People with FMTC have a RET gene mutation but only develop MTC (not other tumors).
If you have the RET gene mutation, you may be able to get preventive surgery to remove your thyroid gland before cancer develops.
Medullary thyroid cancer usually presents as a lump or nodule on your thyroid gland. You may notice it, or your healthcare provider may discover it during a routine neck exam. Sometimes, providers discover it accidentally with imaging tests you get for other reasons.
Your provider will likely recommend the following tests to help diagnose MTC:
Your provider may also recommend genetic testing to see if you have MEN2. If you do, they’ll recommend genetic testing for your biological family members, as well.
The main treatment for MTC is surgery to remove your entire thyroid gland (total thyroidectomy).
If the thyroid cancer has spread (metastasized) to lymph nodes in your neck, your surgeon will likely remove them, as well. After surgery, you’ll need to take thyroid hormone replacement medications for the rest of your life.
Other than surgery, your healthcare provider may recommend other treatments, including:
After treatment for MTC, your provider will check your levels of CEA and calcitonin through blood tests. This way, they can keep track of how well the treatment is working or if the cancer has come back.
MTC is usually more aggressive than the other, more common types of thyroid cancer. It’s easier to treat and manage if it’s found before it spreads to lymph nodes in your neck or other parts of your body.
The prognosis (outlook) for medullary thyroid cancer (MTC) depends on several factors, including:
Advertisement
The prognosis of MTC is usually not as good as papillary and follicular thyroid cancers. But if you and your provider discover MTC early, surgery can cure it. Even if the diagnosis is delayed, MTC often progresses (gets worse) relatively slowly.
A worse prognosis may affect those:
Current research estimates that the five-year survival rate for stages 1 to 3 of medullary thyroid cancer is 93%. It’s 28% for stage 4.
It’s important to note that since there are so few new MTC cases diagnosed each year, these survival rates may not be very accurate. Your healthcare team will give you a better idea of what to expect.
Papillary thyroid cancer is the most common type of thyroid cancer. It represents about 80% of all thyroid cancer diagnoses. Medullary thyroid cancer (MTC) is rare.
Papillary thyroid cancer begins in the thyroglobulin-producing follicular cells in your thyroid. MTC arises from calcitonin-producing cells in your thyroid. Thyroglobulin is a protein, and calcitonin is a hormone.
Advertisement
Papillary thyroid cancer is often linked to radiation exposure, whereas MTC isn’t.
Receiving a cancer diagnosis is unsettling, regardless of the type. Fortunately, medullary thyroid cancer (MTC) generally responds well to treatment if it’s caught early. While most MTC cases have an unknown cause, there’s a significant link to certain inherited conditions. If you or one of your first-degree relatives has been diagnosed with MTC, it’s important to get genetic testing. If you have questions about your risk of developing MTC, talk to your healthcare provider. They’re available to help you.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Hearing you have cancer can be scary. But most thyroid cancer is treatable, and the providers at Cleveland Clinic are here to help.
