Why does chemotherapy cause side effects?
Side effects are common when you’re receiving chemotherapy treatment for cancer. Chemotherapy, or chemo, is a common cancer treatment that uses drugs to damage and destroy fast-growing cells, like cancer cells. The drugs disrupt processes cancer cells need to multiply and thrive. Chemotherapy is a powerful cancer fighter, which is why it’s one of the most common cancer treatments your provider may recommend.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
But there’s a downside. Chemo can’t tell the difference between fast-growing cancer cells and fast-growing healthy cells. When the chemo damages healthy cells, you can experience side effects. The cells most at risk for damage from chemo include:
- Skin cells and hair follicles.
- Cells in your mouth (mucosa), digestive system and reproductive system.
- Blood-forming cells in your bone marrow (white and red blood cells, and platelets).
The good news is that while damaged cancer cells die, normal cells can repair themselves. Most people receive chemotherapy spread out over several sessions, or rounds, to give their cells time to repair. Allowing your body time to recover can make side effects more manageable.
No one can predict what side effects you’ll experience with chemo (or how severe they’ll be). Still, knowing about potential side effects and how to manage them can help you cope with chemotherapy treatments more effectively.
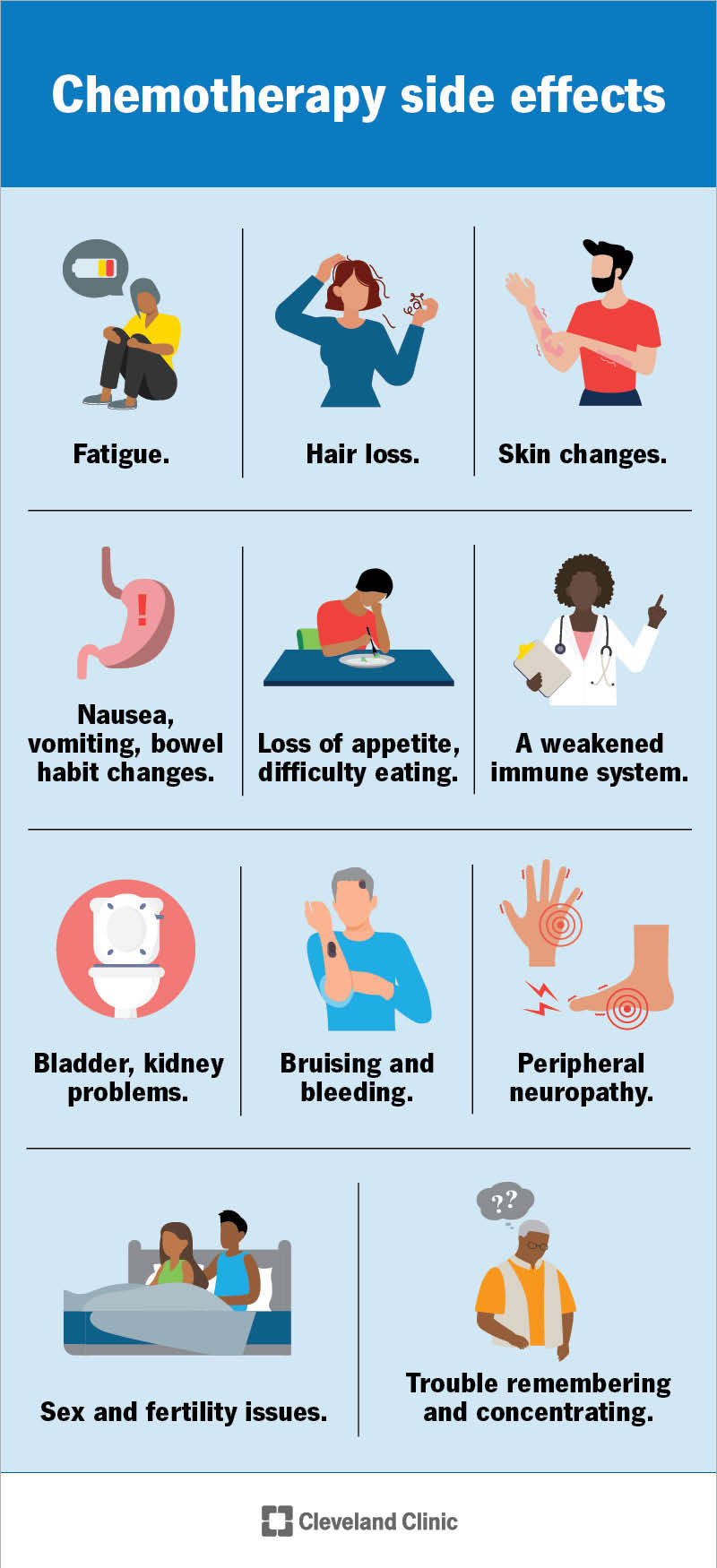
What are the most common side effects of chemotherapy?
The side effects that you experience depend on which normal cells the chemotherapy damages. Much depends on the chemotherapy drugs you’re taking and the dosage. The most common side effects include:
- Fatigue. Fatigue is the most common chemotherapy side effect. The work your body is doing to fight cancer and recover from treatments can leave you feeling drained. Chemotherapy can also cause low blood counts (anemia), which leads to feeling tired.
- Hair loss. Hair usually starts falling out within the first three weeks of starting chemo. Although the hair loss may be permanent, hair usually starts to regrow within two to three months after you finish treatment. It may be a different color or texture than before.
- Skin changes. Chemotherapy can irritate your skin. Rashes, including hand-foot syndrome, are common during chemotherapy. Chemotherapy may also make you sensitive to sunlight, increasing your risk of sunburn.
- Nausea and vomiting. Chemotherapy-induced nausea and vomiting (CINV) affects up to 80% of people who get chemotherapy. It’s likely your gut will feel sick at some point.
- Changes in bowel habits. Chemo can cause constipation and diarrhea. Some people become temporarily lactose intolerant during chemo.
- Loss of appetite. Chemotherapy can change your sense of taste so you don’t want to eat. For example, bitter foods may taste especially bitter. All foods may taste metallic.
- Difficulty eating. Mouth sores and a sore throat, which make it painful to eat, are also common chemo side effects.
- Bladder and kidney problems. Some chemotherapy drugs can make it hard to pee or empty your bladder. You may notice pain or a burning sensation when you pee, you may feel the constant urge to pee, or you may pee or dribble accidentally (urinary incontinence).
- A weakened immune system. Chemotherapy drugs lower your number of white blood cells. This increases your risk of getting sick. People getting chemo are especially at risk of neutropenia. This involves having a low number of cells that help fight infection.
- Bruising and bleeding. Chemo can lower your platelet count. Low platelets (thrombocytopenia) can make injuries bleed more than expected. You may bruise more easily or notice tiny red spots of bleeding underneath your skin (petechiae).
- Peripheral neuropathy. Chemotherapy-induced peripheral neuropathy (CIPN) may make parts of your body (usually your hands and feet) feel painful, numb or tingly (a “pins and needles” feeling). You may find it difficult to coordinate your muscles.
- Trouble thinking and remembering. Chemo brain prevents you from thinking as clearly as you’re used to. Some people going through chemo experience issues with memory, especially short-term memory.
- Sex and fertility issues. Chemo can decrease levels of estrogen and testosterone. This can impact your ability to have children and sex drive. It can lead to early menopause. Some chemotherapy medicines can harm the fetus if you get pregnant or impregnate someone during treatment.
How can I manage chemotherapy side effects?
Your healthcare provider can advise you on what to do to manage the side effects you’re experiencing. In the meantime, there are some tried-and-true management strategies that can help.
Fatigue
To help manage fatigue during and after your chemo rounds:
- Pay attention to your new energy levels. Keep track of when you feel most tired and why. Keep a diary for one week to note your patterns. Understanding your energy levels can help you plan your days more effectively.
- Plan daily activities. Expect to have less energy than you once did for everyday tasks. Given the new limitations, decide which activities take priority and which ones you can delay or get others to help with.
- Balance activity with rest. Balance light daily exercise, like walking, with frequent rest breaks. A short daily nap (30 minutes or less) is a good idea, but don’t sleep so much that you have trouble falling asleep at night.
- Focus on wellness. Eat nutritious foods, get enough exercise and sleep, and manage stress. Speak to a dietitian or a psychologist if you need help planning a wellness routine to help cope with chemo.
Hair loss
To adjust to hair loss:
- Plan for changes beforehand. Have a wig made that matches your hair. Incorporate hats, head wraps or scarves into your wardrobe. Ask your healthcare provider about the “Look Good Feel Better” program, which helps people manage appearance-related side effects of chemo.
- Be gentle with your hair. Avoid frequent shampooing and using styling products that can damage your hair. This includes styling tools that use heat. Use warm water to wash your hair, and gently pat dry with a towel.
- Protect your head and scalp. When you’re outside, wear a cap, turban, scarf or a hat made of soft cotton to protect your head from the elements.
Skin changes
To take extra care of your skin, you should:
- Be gentle with skin care. Avoid applying products that can irritate your skin, like cosmetics, perfumes, powders or harsh, scented creams. Cleanse your skin using lukewarm water and mild soap. Pat your skin dry with a towel instead of rubbing it.
- Protect your skin from damage. Don’t apply direct heat (like heating pads) or cold (like ice packs) to your skin. Don’t apply medical tape or bandages onto affected skin unless your healthcare provider tells you to.
- Use sun protection. Apply sunscreen of SPF 30 or higher and reapply regularly when you’re outside. You can also wear a large-brimmed hat or protective clothing to cover your skin.
- Let your skin breathe. Wear loose clothing made from natural fibers, like cotton.
Nausea, vomiting and changes in bowel habits
To reduce your chance of experiencing digestive system issues (or to minimize their severity):
- Time meals around chemo treatments. Eating immediately before or after getting chemotherapy can increase your risk of nausea. Allow yourself time between treatments for meals.
- Eat mindfully. Eat small, frequent meals throughout the day. Chew slowly to give your body plenty of time for digestion. Avoid foods that are hard to digest, like spicy, fried or high-fat foods. Steer clear of foods that cause gas, as well as dairy if it’s causing diarrhea.
- Drink mindfully. Drink six to eight 8-ounce glasses of fluid daily but do so between meals instead of during. To reduce your risk of stomach upset, drink cold beverages, like flat soda, pulpless fruit juice and flavored drink mixes. Popsicles and gelatin are good options, too.
- Rest and relax. Rest after meals to allow your stomach time to settle.
- Take medications (as prescribed). Your healthcare provider may prescribe medications that can help ease symptoms.
Loss of appetite or difficulty eating
You may need to change how you prepare and consume snacks and meals, so eating doesn’t start to feel like a chore. You can:
- Improve the taste of food. To combat metallic tastes, eat sour fruits or suck on fruit-flavored sourballs. Avoid using metal utensils or cookware. If your taste is dulled, you can experiment with new seasonings, like salad dressings.
- Keep your mouth moist to help with swallowing. Sipping liquids while eating or trying liquid nutritional drinks can help keep your mouth moist. Between meals, suck on ice chips or sugar-free candy. Artificial saliva and Biotene® products can also help.
- Be gentle with mouth sores. Eat soft foods served at room temperature to keep from irritating mouth sores. Avoid carbonated beverages and crunchy or acidic foods (like citrus). Try to avoid coffee, chocolate and alcohol. Your healthcare provider may recommend a soft diet.
Bladder and kidney problems
To help manage or prevent bladder and kidney problems:
- Drink fluids mindfully. Drink six to eight 8-ounce cups of liquid daily, but avoid beverages like coffee and alcohol that increase how often you have to pee.
- Reduce your risk of a urinary tract infection (UTI). Prevent UTIs by taking showers instead of baths, wearing cotton underwear and avoiding tight-fitting pants. Follow your healthcare provider’s instructions about caring for your catheter if you use one.
- Plan trips to the bathroom. Plan bathroom breaks every few hours and take time to pee before exercise and bedtime.
A weakened immune system
To help prevent infections during chemo:
- Get all recommended vaccinations. Protect yourself by staying up to date on all vaccinations.
- Practice good hygiene. Frequent handwashing, wearing clean and dry clothes, and cleaning and bandaging any wounds immediately can reduce your risk of infections.
- Protect yourself from germ spread. Avoid being around people who are sick until they’re better. Mask up if there’s a risk of catching a bacteria or virus that spreads through the air. Cook foods thoroughly to prevent food poisoning.
- Get shots to boost your white blood cells (as recommended). Your healthcare provider may recommend granulocyte-colony stimulating factor (G-CSF) shots. This treatment stimulates your body to make more white blood cells to make up for the ones damaged during chemotherapy.
If you suspect you have an infection and you’re getting chemo, contact your healthcare provider immediately. Signs include fever and chills. Infections during chemo can be serious and even life-threatening.
Bruising and bleeding
To help minimize your risk of bruising and bleeding:
- Try to avoid falls. Take steps to prevent falls both in and outside of your home.
- Try to prevent cuts. Prevent bleeding gums by using a soft toothbrush. Shave using an electric razor to reduce your risk of a cut. Moisturize your skin using mild, unscented moisturizer, and use lip balm to prevent chapped lips. These areas are at risk of bleeding if they get too dry.
- Avoid certain medications. Some over-the-counter medications, like aspirin and ibuprofen increase your risk of bleeding and bruising. Ask your healthcare provider which medications are safe to take.
Contact your healthcare provider immediately if you have bleeding that won’t stop (lasts longer than a few minutes) or if you have blood in your pee or poop. Reach out if you’re bleeding from your vagina when you’re not on your period.
Peripheral neuropathy
Let your healthcare provider know if you’re experiencing symptoms of peripheral neuropathy, like tingling or numbness in your hands or feet. Depending on your symptoms, they may need to adjust your chemotherapy dosage to prevent nerve damage. They may need to prescribe pain medications that can relieve your symptoms.
Trouble thinking and remembering
To help keep your mind and memory sharper:
- See a psychologist or therapist. Attend to your mental health by seeing a mental health provider regularly. Cancer is a major stressor. Mental health care is vital during this time.
- Get enough sleep. Get at least eight hours of sleep each night. Your body (and mind) need this time to repair and refresh.
- Exercise your mind. Exercise your brain by reading regularly, completing puzzles and engaging in other activities that challenge your mind. Ask your healthcare provider to recommend activities.
- Try to stay organized. Reduce the strain on your memory by taking notes and having a set place where you keep them. Organize household items you use most so you can find them easily.
Sex and fertility issues
Intimacy and family planning don’t stop being important just because of a cancer diagnosis. To help with these parts of your life:
- Seek guidance on sex-related issues. Speak with your healthcare provider about challenges in the bedroom. They may be able to recommend medications to improve symptoms like vaginal discomfort or erectile dysfunction. Talking to a sex-positive therapist can also help.
- Plan for pregnancy. Discuss your desire to have children with your healthcare provider before treatment. They can advise you on timing your pregnancy, so it’s safe. They can connect you with resources to help you conceive after treatment, like sperm banking and cryopreservation.
When do side effects start?
Many people experience side effects like fatigue and nausea within a few days of getting chemotherapy. Similarly, when they occur, issues like constipation and diarrhea usually start shortly after chemo. Symptoms often follow a pattern. Usually, they’re worse immediately after getting chemo and gradually improve before the next round of treatment.
Hair loss and fatigue are two notable exceptions. Hair usually starts to fall out within the first three weeks of treatment and doesn’t grow back until after treatment ends. Fatigue often tends to get worse with each progressive round of chemo. This means that if you feel weak after your first chemo session, you’ll likely feel weaker after the second.
Still, there isn’t a set timeline for when chemotherapy side effects start. You may not experience some side effects until the middle or the end of an entire course of treatment. Your experience depends on your overall health and your treatment regimen.
Does your body ever fully recover from chemotherapy?
Most side effects go away within a few months after you finish treatment. It takes about six months to a year for most people to regain their previous energy levels.
Some side effects may linger for months or even years. Others don’t start until after treatment and are long term. Potential long-term chemotherapy treatment side effects include:
- Fatigue. Approximately 15% to 35% of people experience chronic (long-term) cancer fatigue.
- Peripheral neuropathy. Some people experience the lingering effects of peripheral neuropathy for months or years. But for most people, sensation returns gradually.
- Brain fog. Cloudy thinking or trouble remembering may last for several months or years beyond chemotherapy treatment.
- Bone loss: Chemotherapy can make your bones weaker, increasing your risk of osteoporosis and fractures.
Ask your healthcare provider about the likelihood of long-lasting chemotherapy side effects based on your treatment plan. If you’re experiencing side effects that you can’t manage alone, ask them to connect you to palliative care resources that can help. Palliative care isn’t the same as hospice (end-of-life) care. Its purpose is to provide symptom relief and improve your quality of life, no matter your treatment goals.