Gonorrhea, or “the clap,” is a sexually transmitted infection (STI). Often, gonorrhea doesn’t cause symptoms, especially in women. When present, symptoms differ based on your reproductive parts. See your healthcare provider if you think you’re infected. Prompt treatment with antibiotics can prevent long-term problems.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Gonorrhea is a common sexually transmitted infection (STI) that comes from a bacteria called Neisseria gonorrhoeae (N. gonorrhoeae). It’s also sometimes called “the clap” or “drip.” Sexually active people of any age can get gonorrhea and give it to their partners. You can also pass the infection to your baby during childbirth.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
People spread gonorrhea through sexual fluids, including vaginal fluid and semen. You can get gonorrhea from intercourse, anal sex, oral sex or sharing sex toys with an infected person.
Often, gonorrhea doesn’t cause symptoms and you don’t know you have it. This makes it easy to infect your partners accidentally. Getting tested for gonorrhea if you’re sexually active and using condoms or dental dams during sex can reduce your risk of infection.
If you believe you have gonorrhea, don’t wait to seek treatment. Untreated gonorrhea can cause long-term health complications. Your healthcare provider will prescribe antibiotics to clear up a gonorrhea infection.
Gonorrhea is the second most common STI caused by bacteria — just behind chlamydia. Close to 1 million new gonorrhea infections occur in the United States every year. About half of these infections occur in people ages 15 to 24.
Gonorrhea often doesn’t cause symptoms. This is especially the case if you’re female. If you do experience symptoms, they’ll likely impact you differently based on if you have a vagina or penis.
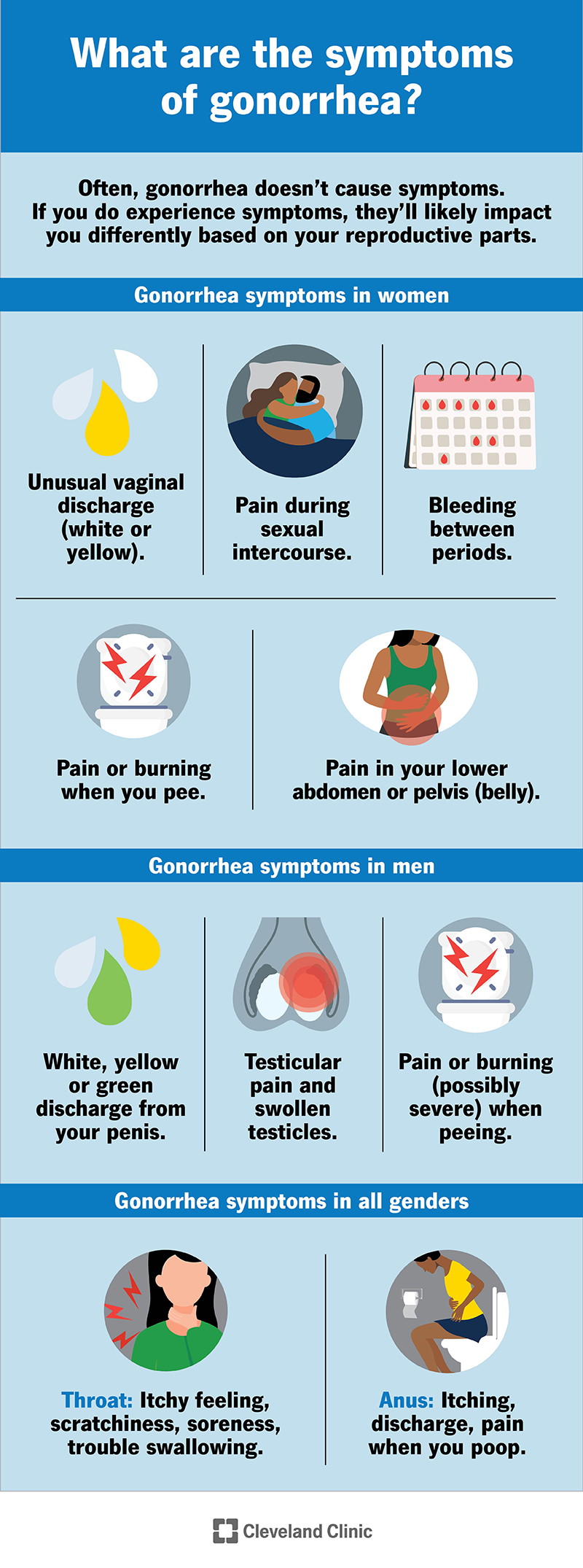
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/4217-gonorrhea.jpg)
Gonorrhea symptoms vary depending on your reproductive anatomy.
Up to 50% of women won’t experience symptoms. This makes it easier to unknowingly pass the infection to your sexual partners. It’s essential to get tested for gonorrhea if you’re sexually active or if you believe you’ve had sexual relations with someone who has gonorrhea.
Advertisement
When symptoms are present, they may include:
Men are more likely to experience symptoms. Still, you may not notice signs of infection until several weeks after exposure, which means you can unknowingly infect partners.
Symptoms may include:
Anyone can get gonorrhea infections in their throat (through oral sex) or rectum (through anal sex). These types of infections are less common than gonorrhea affecting your genitals.
Symptoms may include:
You may not have symptoms of gonorrhea for several weeks after the infection enters your body. Your immune system may not recognize it as an infection right away. On average, most people experience symptoms within two weeks (14 days).
You get an infection when the bacteria that causes gonorrhea (N. gonorrhoeae) enters your body through sexual fluids, like semen or vaginal fluid — often through unprotected sex. The bacteria can enter your body through a penis, vagina, mouth or anus. Neither you nor your partner has to ejaculate (cum) to spread the bacteria. You can also spread gonorrhea by sharing sex toys that haven’t been washed or covered with a new condom.
You can get gonorrhea if you have sex with an infected person. This is the same, no matter your sex. Vaginal intercourse, anal sex, oral sex and sharing sex toys that haven’t been cleaned or protected with a condom can all expose you to the bacteria. Close genital-to-genital contact without penetration can expose you, too.
In women, the most common site of infection is your cervix. In men, infection usually starts in the urethra, the tube that carries pee out of your body.
Gonorrhea is contagious and spreads easily during sexual activity. Still, not all intimate acts or body fluid exchanges put you at risk for gonorrhea. You can’t get gonorrhea from:
You’re at a greater risk of getting gonorrhea if you:
Gonorrhea can cause serious complications when left untreated. If gonorrhea spreads throughout your body it can cause swollen and painful joints, liver inflammation, and heart valve and brain damage. Other complications can depend on your reproductive anatomy.
Advertisement
In women, untreated gonorrhea can:
In men, untreated gonorrhea can cause:
Only a healthcare provider can tell you for sure if you have gonorrhea. First, they’ll ask you questions about your symptoms and sexual history. Then, your provider will collect a sample of your pee or bodily fluid to check it for the bacteria that causes gonorrhea.
Your provider may:
Your provider will discuss which type of gonorrhea test is best in your situation and what kind of fluid sample that test requires. Your provider may also test you for chlamydia. These infections often occur together.
You’ll need antibiotics to treat gonorrhea. Your partner(s) will need treatment, too.
Advertisement
Treatment typically involves one shot (injection) of ceftriaxone. Your provider will determine your dosage based on your weight.
If you’re allergic to ceftriaxone, your healthcare provider may give you a shot of gentamicin plus azithromycin, which is an antibiotic you take orally (by mouth).
Your provider may prescribe additional medication, like doxycycline, to clear a co-infection with chlamydia. Follow your provider’s instructions on what medications to take and when.
It’s important to consider what treatment can and can’t do. Treatment can’t:
It’s important to take preventive steps to protect yourself after treatment so you don’t get re-infected.
Gonorrhea infection clears up within seven to 14 days after treatment with antibiotics. Some healthcare providers recommend a second gonorrhea test to make sure the infection is completely gone. You should avoid sex for the first seven days of treatment so you don’t spread the infection.
Yes. Prompt treatment can cure gonorrhea. Take all medicine as your healthcare provider instructs, even if your symptoms improve and you start to feel better. Also, never take someone else’s medicine to treat your illness.
Advertisement
Taking all antibiotics as prescribed is always important, but it’s especially important with gonorrhea. Gonorrhea is curable now, but it’s becoming more resistant to antibiotics. Some forms of gonorrhea that have developed a high level of antibiotic resistance are commonly referred to as “super gonorrhea.”
To ensure that gonorrhea remains curable, it’s more important than ever that everyone takes medications as prescribed — and that everyone takes steps to prevent infection.
People who get prompt treatment and follow treatment instructions can resume their normal lives within one to two weeks. Untreated gonorrhea can cause several long-term health problems.
You can get gonorrhea more than once, so taking steps to avoid getting it and spreading it again is important. Ask your healthcare provider about getting regular STI tests. Additionally, you should practice safe sex like using condoms every time you have sex and being open with your sex partners about your sexual history.
Talk to your pregnancy care provider. You can spread the infection during delivery, which can cause health problems for your newborn. Babies born to parents with untreated gonorrhea are at risk for complications like low birth weight and blindness.
Your provider will help you get the right testing and treatment to keep you and your baby safe.
The only way to prevent gonorrhea is not to have sex. For many people, a more realistic goal is to reduce the risk of contracting and spreading gonorrhea. Take these steps to reduce your risk:
There’s no perfect protection for gonorrhea if you’re sexually active. For instance, condoms can tear. Still, taking extra precautions during sex can greatly reduce your risk of infection.
The Centers for Disease Control and Prevention (CDC) recommends that all women who are sexually active and under 25 get tested for gonorrhea each year. Regardless of sex, you may need to get tested annually if you’re considered high risk for contracting gonorrhea. Your risk factors include your age and sexual activity. People who are in a long-term relationship with only one sex partner may not need testing as frequently. Talk to your healthcare provider about how often you should get tested based on your risk.
Your healthcare provider will give you instructions about when you can resume sex. Typically, you need to wait at least a week after you and your partner(s) finish all your medications before having sex.
If you’re sexually active and at a higher risk for gonorrhea, consider regular STI testing. Since many STIs, including gonorrhea, don’t cause symptoms, you could have an infection and pass it on to others without knowing it. Untreated gonorrhea can also cause complications that you can avoid with regular testing and prompt treatment.
If you have gonorrhea, questions you may want to ask include:
Gonorrhea often doesn’t cause symptoms, especially in women. You can have it for several weeks or months and not know.
It’s possible that you can have gonorrhea, but your partner doesn’t. There are a few reasons that could happen. For example, they could have it unknowingly because the infection may not be causing symptoms. Or they could have a re-infection, which means a past infection wasn’t completely cured and came back.
Gonorrhea is a very common STI, but it doesn’t mean it’s unavoidable. The best way to prevent gonorrhea is to get tested for the infection and use a condom or dental dam during any sexual activity. Safer sex is especially important with gonorrhea since it often doesn’t cause symptoms. If there’s a chance you’ve been exposed, don’t let embarrassment prevent you from scheduling a visit with your healthcare provider. Get tested immediately. Untreated gonorrhea can cause long-term damage to your health. You don’t have to face these complications, especially when a simple course of antibiotics can cure the infection.
Learn more about the Health Library and our editorial process.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Cleveland Clinic's health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability, and up-to-date clinical standards.
Don’t ignore sexually transmitted infections. Cleveland Clinic experts will treat them confidentially and quickly in a judgment-free environment.
