Bronchiectasis is a condition where damage causes the tubes in your lungs (airways) to widen or develop pouches. It makes it hard to clear mucus out of your lungs and can cause frequent infections. Coughing a lot with pus and mucus is the main symptom of bronchiectasis. Bronchiectasis can’t be cured but can be managed with treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
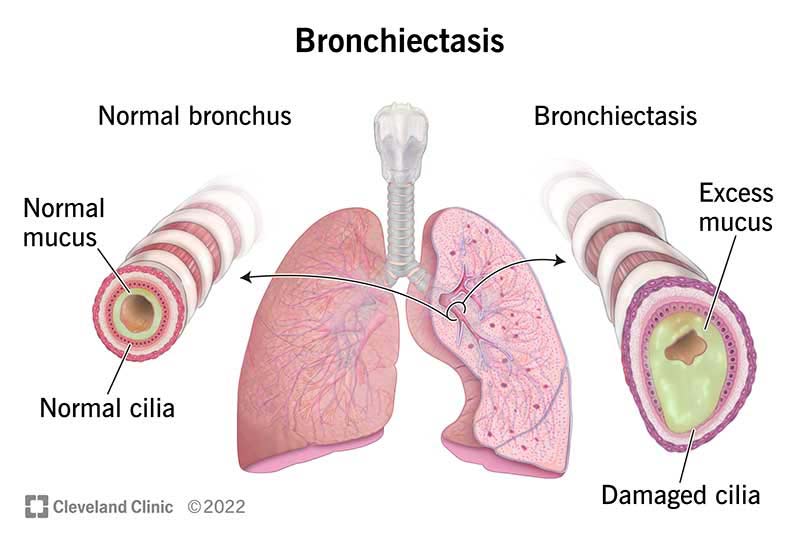
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/21144-bronchiectasis)
Bronchiectasis (“bronk-ee-EK-tuh-sis”) is a lung condition where your airways (tubes going into your lungs) get damaged and widen. Damaged airways can’t clear mucus like they're supposed to. Bacteria then grows in the mucus, causing more inflammation and damage to your lungs. This makes you cough a lot as your body tries to remove the infected mucus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Bronchiectasis and bronchitis have similar symptoms, including mucus in your lungs and coughing. But bronchiectasis causes permanent widening of your airways and bronchitis is a temporary infection that doesn’t cause lasting damage.
Healthcare providers categorize bronchiectasis based on what the damage to your airways looks like — cylindrical (or tubular), varicose or cystic. Cylindrical bronchiectasis is the most common and least serious form of bronchiectasis. Cystic bronchiectasis is the most severe form.
Providers also categorize bronchiectasis as focal (in one area) or diffuse (in many areas throughout your lungs). Traction bronchiectasis happens when scarring in your lungs pulls your airways out of shape.
You’re at higher risk of bronchiectasis if you’re living with an underlying condition that affects your lungs or immune system. Without an underlying condition, your risk increases as you get older.
About 350,000 to 500,000 people in the U.S. have bronchiectasis. This includes one person out of 150 people who are 75 and older. The actual number might be higher since you can have bronchiectasis without having any symptoms.
The tubes (airways or bronchi) going into your lungs have defenses to protect you from disease. Annoying as it can sometimes be, mucus is one of these defenses. When mucus can’t be coughed out, it causes lasting damage to your airways.
Advertisement
When you breathe air in, any harmful particles get trapped in mucus in your airways. Then, millions of tiny, hairlike structures (cilia) use a coordinated motion to move the mucus out of your lungs, like waves bringing debris to the shore. This is called mucociliary clearance. You cough out the mucus or swallow it, where the trapped particles are destroyed by your stomach acid.
When any part of this system isn’t working — if your cilia are damaged or your airways have pockets that trap mucus — you build up mucus in your lungs. The mucus has bacteria trapped in it, which can multiply and cause infections. The damage the infections causes can make bronchiectasis worse.
Bronchiectasis can be mild or severe depending on how much damage you have in your lungs. Some people have it and don’t even know it. Others have had it for a long time and repeated infections have severely damaged their lungs. Most people with bronchiectasis live a normal life span by manage their symptoms with a provider’s advice and medication.
Symptoms of bronchiectasis include:
You might have stretches of time where your symptoms aren’t as bad and then have a flare-up (exacerbation) where your symptoms get worse. Exacerbation symptoms include:
Bronchiectasis is caused by two phases of airway damage. In the first phase, the initial damage (or “insult”) is caused by an infection, inflammatory disorder or another condition that affects your lungs. Healthcare providers don’t know the initial cause in up to 40% of people with bronchiectasis.
The first insult makes you more likely to get inflammation and repeated infections that cause further damage to your lungs. This is the second phase, or the “vicious cycle.”
Some of the specific causes of the initial damage (“insult”) which starts the cycle of bronchiectasis include:
Advertisement
Research suggests that COVID-19 isn’t a very common cause of bronchiectasis. But if you’ve had acute respiratory distress syndrome (ARDS) with COVID-19, you may have pseudobronchiectasis. Pseudobronchiectasis looks like bronchiectasis, but it resolves over time rather than causing the cycle of repeated infections and lung damage.
The most common cause of bronchiectasis depends on where you live. In the U.S. and other western countries, the most common cause of bronchiectasis is cystic fibrosis. Worldwide, it’s tuberculosis. In many cases, healthcare providers can't determine the cause of bronchiectasis.
A healthcare provider will diagnose bronchiectasis by examining you and asking you about your health history. They’ll listen to your lungs and test how well they’re working. If they think you have bronchiectasis or another lung condition, they’ll order imaging tests to look at the structure of your lungs.
A healthcare provider may perform a number of tests to diagnose bronchiectasis or rule out other conditions, including:
Advertisement
Bronchiectasis can’t be fully cured, but you can treat the symptoms. Healthcare providers treat bronchiectasis by clearing mucus and managing infections. Depending on the severity of your condition, your provider might prescribe medication or physical therapy. You may also use medical devices that help get rid of mucus.
If bronchiectasis is caused by an underlying condition, treating that condition may help your symptoms. If you have a small area of bronchiectasis, your provider might recommend surgery, though this is rare.
Bronchiectasis treatments help get rid of infected mucus, kill bacteria and decrease inflammation. They include:
Advertisement
What you eat doesn’t seem to directly impact bronchiectasis. For instance, you may have heard that avoiding things like milk can help lower the amount of mucus in your lungs, but research hasn’t shown this to be true.
What’s most important is to maintain good nutrition. You might find yourself losing an unhealthy amount of weight or have other concerns about your diet. Ask for a dietitian if you have concerns about healthy eating with bronchiectasis.
Bronchiectasis can’t be cured — the damage it causes is irreversible. But most people can manage the symptoms of bronchiectasis with strategies recommended by their healthcare provider.
Your outlook will depend on how severe your condition is, how well you respond to treatment and what other health conditions you have. You may need to practice physical therapies or take medications daily. More severe cases may impact your quality of life.
Damage caused by severe bronchiectasis can lead to life-threatening complications, including:
With proper treatment, most people with bronchiectasis can expect to live as long as someone without it. A history of smoking and low lung function can lower your life expectancy.
You can reduce your risk of developing bronchiectasis by managing your lung health:
Talk to your healthcare provider if you’ve been coughing with a lot of mucus for several weeks or if you feel short of breath.
If you have been diagnosed with bronchiectasis, you should contact your healthcare provider if you:
Go to the ER if you are:
In most cases, bronchiectasis shouldn’t keep you from living a full life. Talk to your provider about bothersome symptoms and how to deal with exacerbations. They may not be able to take care of every symptom, but sometimes small changes can greatly improve your quality of life.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Recurrent pneumonia, shortness of breath and coughing up mucus are three big signs of bronchiectasis. Cleveland Clinic is here to help you breathe easier.
