While not everyone with diabetes will develop diabetes-related retinopathy, it’s still a major risk factor for vision loss. But diabetes and diabetes-related retinopathy are both manageable. Combining regular medical care and your own efforts can go a long way to maintaining your vision.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
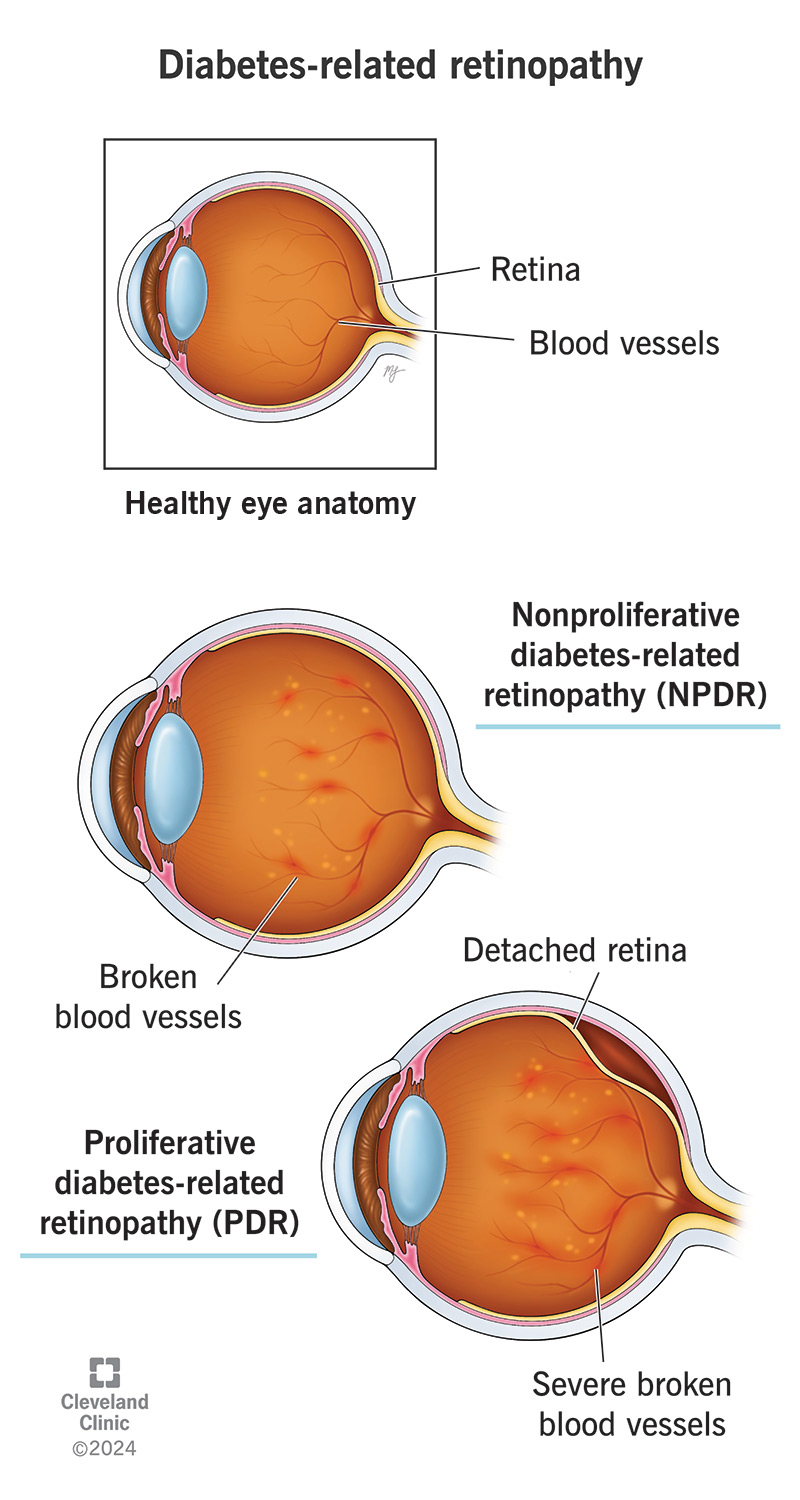
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/diabetes-related-retinopathy)
You might not have symptoms in the early stages of diabetes-related retinopathy. That’s because this condition doesn’t start causing vision changes until the damage is more severe or widespread throughout your retina.
Advertisement
Diabetes-related retinopathy symptoms can include:
Diabetes-retinopathy can happen because of multiple types of diabetes. They include:
Diabetes causes increased blood sugar levels and can damage the insides of blood vessels throughout your body over time. When you have diabetes-related retinopathy, damaged blood vessels in your retina are trying to repair and reroute to avoid an interruption in blood supply. As a result, fragile new blood vessels grow on the surface of your retina. These new blood vessels can cause retinal detachments and bleeding into the vitreous, a gel-like fluid in your eye. The damaged blood vessels can also leak fluid into your retina, causing macular edema. This can cause blurry vision.
Risk factors for diabetes-related retinopathy include:
Complications of diabetes-related retinopathy include:
Eventually, complications of diabetes-related retinopathy can cause so much damage that the light-detecting cells, known as photoreceptors, stop working correctly. When that happens to enough photoreceptors, it causes permanent vision loss and can eventually lead to blindness.
Many of the key changes that happen with diabetes-related retinopathy don’t cause symptoms until much later. But they’re still visible very early on to an eye care specialist who looks at the back of your eyes using special instruments during a dilated eye exam.
Those changes can include:
Diabetes-related retinopathy is treatable but not curable. Some of the symptoms or retinal changes are treatable. But certain types of damage aren’t reversible once they become severe enough.
Advertisement
The two main approaches are managing your diabetes and eye treatments. Your provider will recommend treatments for both of them.
Research clearly ties higher blood sugar and hemoglobin A1C levels to diabetes-related retinopathy. So, managing your blood sugar — keeping it lower and more consistent — is critical to delaying and slowing how diabetes-related retinopathy progresses and affects your retinas.
Key parts of managing your diabetes include:
Advertisement
Eye treatments focus on managing vision and eye symptoms and limiting or slowing retinal damage. Some specific treatments for diabetes-related retinopathy include:
If you have diabetes or diabetes-related retinopathy, it’s crucial that you see an eye care specialist regularly. They’ll recommend a schedule for regular follow-up visits, which can make a big difference when it comes to catching more serious changes before they’re severe or permanent.
You should also call or see your provider if you notice any gradual vision changes like:
Advertisement
You should go to the nearest hospital or emergency room if you have SUDDEN vision changes like:
Diabetes-related retinopathy is a permanent, lifelong condition. There isn’t a cure, but you can take steps to manage it and limit loss of vision.
Diabetes-related retinopathy is likely to happen to people with diabetes, but having diabetes doesn’t guarantee you’ll develop it. Still, it’s important to do everything you can to avoid or delay it because it can so heavily impact your life.
With early diagnosis and timely treatment, you may be able to prevent vision loss and delay diabetes-related retinopathy progression. After diabetes-related retinopathy treatment, you’ll have the best chance of limiting or delaying the effects of this disease if you manage your diabetes and keep your blood sugar within ranges that your providers recommend.
Unfortunately, some people will still develop more severe complications. But there are ways to delay those complications as long as possible and manage diabetes-related vision changes. Anything you can do to limit the severity of any vision changes is preferable to developing more severe issues or changes early on.
Yes, managing your blood sugar levels and maintaining a low hemoglobin A1C can help you prevent diabetes-related retinopathy. Doing these can also make retinopathy regress over time.
Not everyone with diabetes has it, but the odds of developing diabetes-related retinopathy are significantly higher in people with unmanaged blood sugar levels and in people who have diabetes over a longer period of time.
If you don’t have diabetes but have a high chance of developing it (such as having prediabetes), you can act long before you might receive a diabetes diagnosis. Acting earlier can prevent and delay when or if you develop diabetes, which can affect when or if you develop diabetes-related retinopathy.
Eye exams can catch early signs of diabetes-related retinopathy long before you have symptoms. If you have other family members, especially first-degree biological relatives (parents, siblings or children) with diabetes, you have a much higher risk of having it, so regular eye exams are especially important for you.
No matter how well you manage your diabetes, sometimes, it isn’t enough to prevent diabetes-related retinopathy from happening. Managing your diabetes and regular vision exams and eye care are still key, though. They can help you maintain and preserve your vision.
Your diabetes-related healthcare provider can guide you on this and refer you to an eye specialist. With regular care and support, there’s a lot you can do to safeguard your vision.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Your eyes are one of your most important senses. If something goes wrong, it can change your world. Cleveland Clinic can help treat all types of retinal disease.
