The Glasgow Coma Scale is a tool that healthcare providers use to measure decreases in consciousness. The scores from each section of the scale are useful for describing disruptions in nervous system function and also help providers track changes. It’s the most widely used tool for measuring comas and decreases in consciousness.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
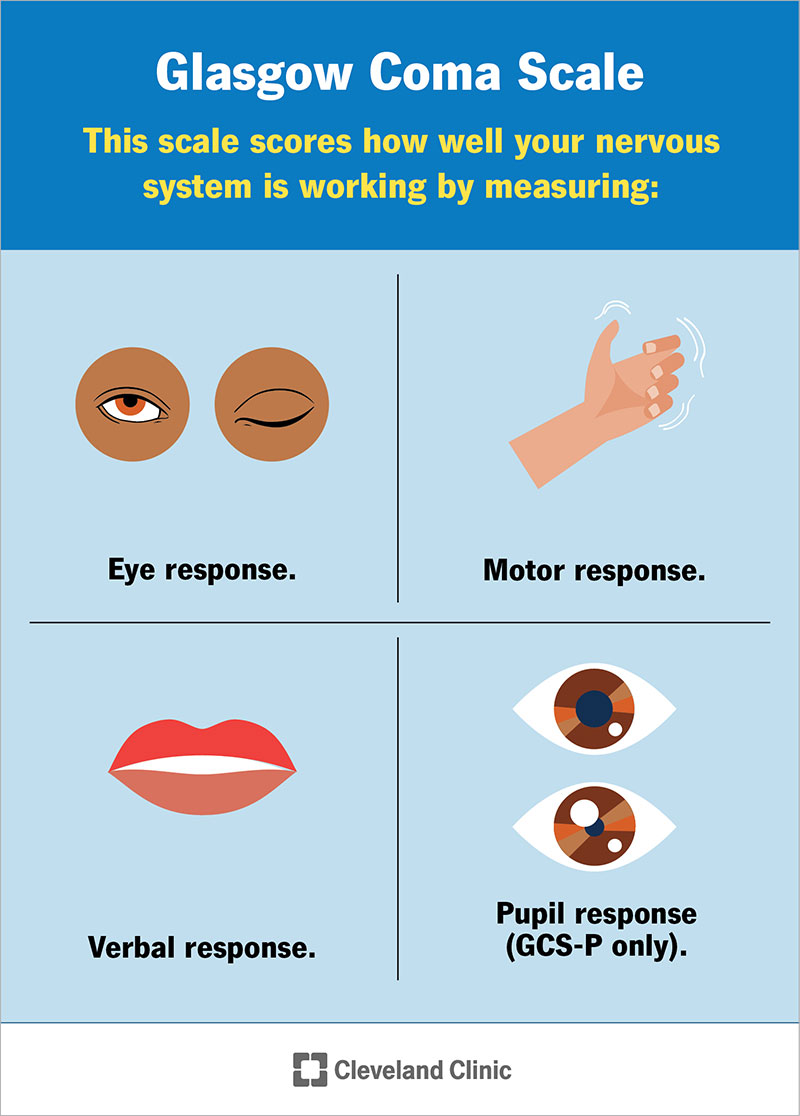
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24848-glasgow-coma-scale)
The Glasgow Coma Scale (GCS) is a system to “score” or measure how conscious you are. It does that by giving numbered scores for how awake you are, your level of awareness and how you respond to basic instructions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Experts at the University of Glasgow in Scotland developed the GCS in 1974. Despite “coma” being part of the name, the GCS sees much wider use in medicine today. It’s the most commonly used scale for measuring decreases in consciousness, including coma.
In the medical context, consciousness has three requirements. To be conscious, you have to be:
Healthcare providers can use the GCS as part of a neurological exam. It’s also useful for any situation where you might have a decrease in how conscious you are. That includes injury-related conditions like concussions and traumatic brain injuries.
The scale also can help with conditions that don’t involve injuries, such as low blood sugar (hypoglycemia), poisoning or after a seizure.
A neurological exam looks for any problems with the function of the two main parts of your nervous system. Those parts are your:
Advertisement
The Glasgow Coma Scale has three categories that apply to a neurological exam. Most of them apply to your brain itself, but some can also involve your spinal cord and nerves throughout your body:
To get your Glasgow Coma Scale score, providers take the scores from the three categories of the GCS and add them together. A healthcare provider will test each of the three categories in multiple ways. An example of this is testing your verbal response by asking you a few different questions, such as what day of the week or date it is or what city you're in currently.
One of the best uses of the GCS is to track changes in your level of consciousness. Healthcare providers will often repeat a neurological exam at regular intervals to check for and document any changes in your GCS score.
The scoring guidelines for the categories are as follows:
This is mainly about how awake you are. If you’re unconscious, it measures the level of unconsciousness by testing reflex responses to pressure. Pressure here means something like a pinch or a poke. It should be just enough to cause minor, momentary discomfort but not injury.
| Eye response score | Score meaning |
|---|---|
| 4 | You can open your eyes and keep them open on your own. |
| 3 | You only open your eyes when someone tells you to do so. Your eyes stay closed otherwise. |
| 2 | Your eyes only open in response to feeling pressure. |
| 1 | Your eyes don’t open for any reason. |
| Eye response score | |
| 4 | |
| Score meaning | |
| You can open your eyes and keep them open on your own. | |
| 3 | |
| Score meaning | |
| You only open your eyes when someone tells you to do so. Your eyes stay closed otherwise. | |
| 2 | |
| Score meaning | |
| Your eyes only open in response to feeling pressure. | |
| 1 | |
| Score meaning | |
| Your eyes don’t open for any reason. |
A provider checks this by asking you questions that test your memory, thinking ability and your awareness of the world around you. Your provider can also use this to see if there are any brain or nerve problems affecting control of your face and mouth.
| Verbal response score | Score meaning |
|---|---|
| 5 | You’re oriented. You can correctly answer questions about who you are, where you’re at, the day or year, etc. |
| 4 | You’re confused. You can answer questions, but your answers show you’re not fully aware of what’s happening. |
| 3 | You can talk and others can understand words you say, but your responses to questions don’t make sense. |
| 2 | You can’t talk and can only make sounds or noises. |
| 1 | You can't speak or make sounds. |
| Verbal response score | |
| 5 | |
| Score meaning | |
| You’re oriented. You can correctly answer questions about who you are, where you’re at, the day or year, etc. | |
| 4 | |
| Score meaning | |
| You’re confused. You can answer questions, but your answers show you’re not fully aware of what’s happening. | |
| 3 | |
| Score meaning | |
| You can talk and others can understand words you say, but your responses to questions don’t make sense. | |
| 2 | |
| Score meaning | |
| You can’t talk and can only make sounds or noises. | |
| 1 | |
| Score meaning | |
| You can't speak or make sounds. |
This part can reveal any issues with the connections between your nerves, spinal cord and brain. It also tests your brain’s ability to control muscle movement and how well you can understand and follow instructions.
| Motor (movement) response score | Score meaning |
|---|---|
| 6 | You follow instructions on how and when to move. |
| 5 | You intentionally move away from something that presses on you. |
| 4 | You only move away from something pressing on you as a reflex. |
| 3 | You flex muscles (pull inward) in response to pressure. |
| 2 | You extend muscles (stretch outward) in response to pressure. |
| 1 | You don’t move in response to pressure. |
| Motor (movement) response score | |
| 6 | |
| Score meaning | |
| You follow instructions on how and when to move. | |
| 5 | |
| Score meaning | |
| You intentionally move away from something that presses on you. | |
| 4 | |
| Score meaning | |
| You only move away from something pressing on you as a reflex. | |
| 3 | |
| Score meaning | |
| You flex muscles (pull inward) in response to pressure. | |
| 2 | |
| Score meaning | |
| You extend muscles (stretch outward) in response to pressure. | |
| 1 | |
| Score meaning | |
| You don’t move in response to pressure. |
In 2018, a team of experts — including one of the original creators of the GCS — published an updated version of the GCS called the “GCS-P.” The P stands for “pupil,” as in the pupil of the eye. This is a fourth number that providers subtract from the standard GCS score.
Advertisement
Pupil reaction is important because it’s an indicator of your brain function. When your pupils don’t react to light, it’s a sign that a serious problem or injury is affecting your brain. The pupil score ranges from 0 to 2.
The pupil scores mean:
Subtracting the pupil reaction score from the GCS score means that the GCS-P score can range from 1 to 15. The GCS-P score still uses a score of 8 or fewer to mean a coma.
A GCS score of 3 and a pupil score of 2 is a GCS-P score of 1. That means a very deep coma and no pupil reaction in both eyes.
Older descriptions of the GCS use the word “pain” to describe the sensation used to test certain reflexes. Newer guidelines change that word to “pressure.” The word change is more accurate because it doesn’t involve an injury. It’s also clearer because a provider isn’t actually trying to cause pain or hurt your loved one.
The original GCS guidelines were also vague on where providers should press to test reflexes. In 1975, a year after the original publication of the GCS, the experts who created the GCS published specific guidance. Points where a provider will put pressure include your:
Advertisement
The highest possible GCS score is 15, and the lowest is 3. A score of 15 means you’re fully awake, responsive and have no problems with thinking ability or memory. Generally, having a score of 8 or fewer means you’re in a coma. The lower the score, the deeper the coma is.
Healthcare providers may abbreviate your GCS score using letter/number combinations. A score of 15 would be “E4V5M6.” A score of 3 would be “E1V1M1.”
When providers use the GCS in connection with a head injury, they tend to apply scoring ranges to describe how severe the injury is. The ranges are:
Generally, your family or close loved ones will be the ones to talk to your healthcare provider about your score(s). Some things you should know about the GCS and how healthcare providers use it include:
Advertisement
The Glasgow Coma Scale is the most common tool healthcare providers use to measure decreases in consciousness and comas. Since its creation almost 50 years ago, experts have studied the scale extensively and found that it continues to be a useful diagnostic tool. (They’ve even improved it along the way.) Using this tool also helps providers track changes in brain function. That helps guide treatment and improve care for people with conditions that affect their level of consciousness.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
If you have a neurological condition, you want expert advice. At Cleveland Clinic, we’ll work to create a treatment plan that’s right for you.
