An opioid overdose happens when opioids disrupt your brain’s ability to regulate breathing. It can cause respiratory failure (stopped breathing). It may be fatal without quick treatment. Naloxone and immediate medical care may prevent life-threatening outcomes. Help is also available for opioid use disorder.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An opioid overdose happens when opioids overwhelm the part of your brain that controls breathing. This can slow or stop breathing. It may lead to death if not treated in time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An overdose can occur if you take too much of an opioid or mix it with other addictive substances. Any opioid, either prescription or nonprescription, can lead to an overdose. The amount that’s “too much” varies based on your tolerance and the strength of the opioid. That can make it hard to know what’s safe and what’s not. So, it’s important to follow prescribing instructions closely or avoid substances when you might not know what the dosage is.
An overdose is a medical emergency. While this is a frightening event, knowing what to do can save a life. An emergency opioid overdose reversal medication may treat the condition if given quickly. But medical care is still needed after emergency treatment to check for complications.
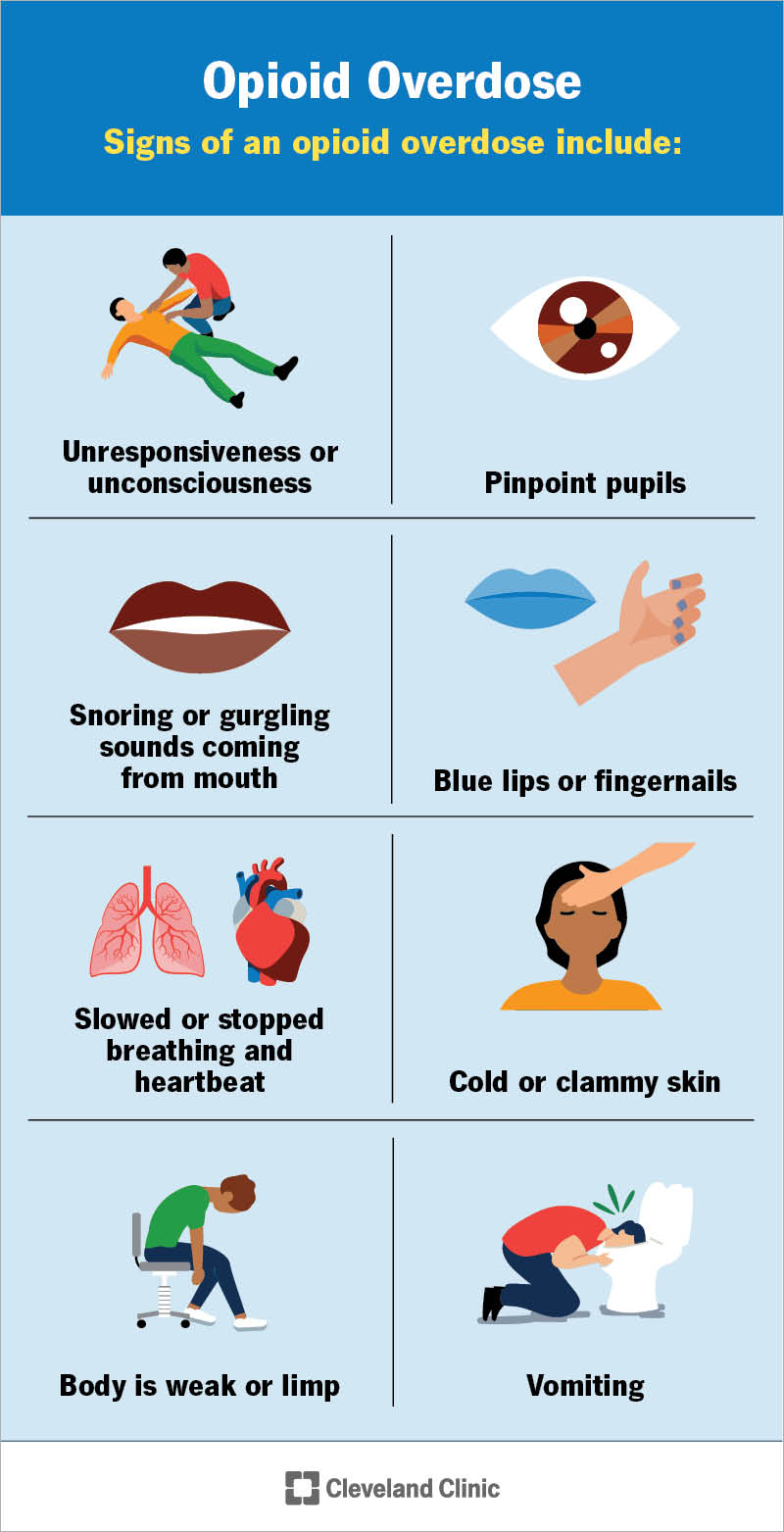
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/24583-opioid-overdose)
Signs and symptoms of an opioid overdose include:
Act quickly if you notice these signs. If you carry an emergency opioid overdose reversal medication, administer it immediately. Then, contact 911 or your local emergency services number.
Advertisement
Taking opioids in a way your body isn’t used to can lead to an overdose. Common examples include:
Anyone who uses opioids could potentially experience an overdose. An overdose can happen if this is your first time using an opioid or if you’ve taken one frequently.
Your risk increases if you:
Research shows that if you had one overdose, you’re at an increased risk of having another in your lifetime.
It can be hard to know what you’re getting when using nonmedical opioids. Because they’re not regulated, their strength can vary. They might be mixed with other drugs like heroin, fentanyl or carfentanil (an extremely potent drug used to sedate large animals). These unknown ingredients increase your risk of overdose and death. Also, pills that are given to you or bought from a friend may look like a safer drug, but might contain lethal doses of nonmedical opioids, including fentanyl.
Opioids bind to receptors in your brain. These receptors are supposed to send signals to the rest of your body to tell it to keep breathing. Opioids interrupt these signals. This causes your breathing to slow and eventually stop (respiratory failure). Your body needs oxygen to survive. Within minutes of not receiving enough oxygen, your brain cells begin to die.
Treating an overdose as soon as possible prevents death and other serious complications like severe disability or brain damage.
First responders or healthcare providers look for signs of an overdose and rely on information from friends and loved ones. As you’re likely unconscious while experiencing an overdose, they’ll assess the scene and look for clues or substances near you.
If first responders suspect an overdose, they’ll administer naloxone. This is an emergency medication that treats opioid overdoses. If your symptoms improve with this medication, it confirms that you had an overdose.
In a hospital setting, providers may order drug tests to make a diagnosis. They’ll also perform other tests to assess your health and look for other signs, symptoms or medical conditions that may need treatment.
Naloxone (Narcan®) and nalmefene are the primary emergency treatments for an overdose. These medications:
Advertisement
Naloxone only works for about 30 to 90 minutes. But overdose effects can return once it wears off. You may need to give an additional dose of the emergency opioid overdose reversal medication as you wait for emergency services to arrive.
Nalmefene is only used in healthcare settings outside the U.S.
Once at the hospital, providers may also perform additional treatments, like intubation, to help you breathe.
Here are some ways to lower the risk of overdose:
If you or a loved one is at risk of overdose, reach out for help. There are medical resources available so you can get the care you need.
If you think someone is having an overdose:
Advertisement
Experiencing or witnessing an opioid overdose can be terrifying. You’re not alone — whether you need to talk to someone about what’s happened or you’re looking for treatment for opioid use disorder. Support groups and treatment programs can help you regain your health and support your future safety. If you have questions or concerns, reach out to a healthcare provider or someone you trust. They’re here to help.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Whether you need stitches, a broken bone set or think your appendix might be causing your abdominal pain, Cleveland Clinic’s emergency medicine team is here to help.
