A blood clotting disorder is a condition that makes your body more likely than normal to make blood clots. You can inherit or acquire one of these conditions. Even if you have a blood clotting disorder, you may not get a bad blood clot like one that causes a stroke. Medicines can keep your blood from clotting too much.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A blood clotting disorder makes your blood form clots too easily. This is also called a hypercoagulable state or thrombophilia.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When you get hurt, your body stops the bleeding by forming a blood clot. Clotting factors (proteins) your liver makes stick to platelets in your blood to form a blood clot (coagulate). Normal coagulation is important for stopping a cut from bleeding and starting the healing process.
However, too much clotting can cause problems.
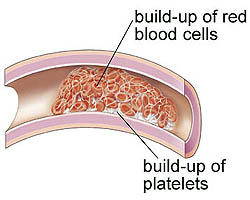
Image content: This image is available to view online.
View image online (https://my.clevelandclinic.org/-/scassets/images/org/health/articles/blood-clotting-thrombusformation2.ashx)
Yes, blood clotting disorders can be dangerous, especially when you don’t get treatment. People with coagulation disorders have an increased risk of getting a blood clot in their:
Another name for a clot inside a blood vessel is a thrombus or an embolus.
Blood clots in your veins can travel through your bloodstream and cause:
Blood clots in your arteries can increase your risk for:
Yes, it’s possible to have a miscarriage if you have a blood clot disorder like antiphospholipid syndrome. This disorder increases your blood clot risk, especially if you’ve had blood clots before. Higher blood volume and pressure during pregnancy play a role in making you five times more likely to develop a blood clot, even if you don’t have a blood clotting disorder.
Advertisement
Factor V Leiden and prothrombin gene mutation (G20210A) are the most commonly identified genetic defects that increase your risk for blood clotting.
About 3% to 8% of people with ancestors from Europe have a copy of the factor V Leiden mutation. Only 1 in 5,000 people has two copies of the mutation.
About 1 in 50 white people in America and Europe have the prothrombin mutation.
Both of these mutations are less common in other populations.
Blood clotting disorder symptoms can vary depending on where in your body you have a blood clot.
Symptoms may include:
Hypercoagulable states are usually genetic (inherited from parents) or acquired conditions.
The genetic form of this disorder means you’re born with the tendency to form blood clots.
Acquired conditions are usually a result of surgery, trauma, medications or a medical condition that increases the risk of forming clots.
Certain conditions increase your risk of developing blood clots. However, that doesn’t mean you have a genetic hypercoagulable state. That’s why your healthcare provider will do a careful evaluation of your personal and family medical history.
Advertisement
You may be a candidate for screening for coagulation disorders if you have:
Blood tests can help your healthcare provider evaluate your condition.
Blood clot disorder tests include:
Some of the tests help detect conditions that can be associated with hypercoagulable states.
Tests used to help diagnose inherited coagulation disorders include:
Advertisement
Other tests that help diagnose acquired coagulation disorders include tests for:
Testing can help:
A specialized coagulation laboratory should do the tests. A pathologist or clinician with expertise in coagulation, vascular medicine or hematology should interpret them.
Ideally, the tests should be done when you aren’t having an acute clotting event.
In most cases, you only need blood clotting disorder treatment when a blood clot develops in a vein or artery. Anticoagulants decrease your blood’s ability to clot and prevent additional clots from forming.
Anticoagulant medications include:
Advertisement
Your healthcare provider will talk to you about the benefits and risks of these medications. This information, along with your diagnosis, will help determine the type of anticoagulant medication you will take, how long you will need to take it, and the type of follow-up monitoring you need.
As with any medication, it’s important to know how and when to take your anticoagulant according to your provider’s guidelines and to have frequent blood tests. You shouldn’t take warfarin if you're pregnant or planning to become pregnant. If you are, ask your provider about switching to a different type of anticoagulant medication, especially during the first trimester and before delivery.
Ask your healthcare provider about specific dietary guidelines you'll need to follow while taking warfarin. Certain foods, such as foods high in vitamin K, can change the way the medication works. These include:
Side effects of anticoagulants may include:
If you're taking warfarin:
You can manage blood clot disorders by taking medicine and going to follow-up appointments with your healthcare provider. If you’re planning to have surgery or become pregnant, talk with your provider about how to stay safe during these times.
If you inherited your blood clotting disorder from your parents, you’ll have it for the rest of your life. Although that doesn’t mean you’ll get a blood clot, there may be times in your life when an additional risk factor increases the risk you already have.
Many acquired coagulation disorders go away when the situation that caused them goes away. For example, when you’re up and moving again after a long plane ride, your risk of clots goes back down.
If you’re born with an inherited form of blood clotting disorder, you can’t prevent it. Still, that doesn’t mean you’re going to get a blood clot.
Possible ways to prevent an acquired blood clotting disorder include:
If you’re taking warfarin, you may bleed or bruise more easily when you’re injured. Call your provider if you experience heavy or unusual bleeding or bruising.
Contact your provider if you think you have deep vein thrombosis.
Call 911 if you think you’re having a pulmonary embolism because you have chest pain and difficulty breathing. Heart attack and stroke are other medical conditions that need emergency treatment.
If you have a blood clotting disorder, be sure to stay in touch with your healthcare provider. Take any medicine they prescribe for you and keep going to your follow-up appointments. Let them know if you’re planning to become pregnant or have surgery. And ask first before taking any medicine you buy without a prescription. Your provider is on your side and wants to help you, so don’t be afraid to ask questions about your condition.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about the Health Library and our editorial process.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Cleveland Clinic’s health articles are based on evidence-backed information and review by medical professionals to ensure accuracy, reliability and up-to-date clinical standards.
Blood clotting disorders can be genetic (inherited) or acquired. Cleveland Clinic’s experts diagnose and treat these disorders to lower your risk of complications.
